Verification of Benefits With Hansei Solutions
Hansei Solutions offers verification of benefits to help behavioral healthcare providers verify insurance coverage and eligibility for their patients, reducing the risk of denied claims and increasing overall revenue.
Advanced Eligibility & Benefits Verification
Verification of benefits, or VOB, is the first step in claims and revenue cycle management, ensuring accurate payment from insurance companies. However, with the increasing number of new addiction and mental health treatment providers, insurance providers are paying out fewer claims, making the VOB process more challenging.
As insurance providers add more criteria to their benefit plans, the administrative tasks involved in VOB can become burdensome. Hansei Solutions aims to address this problem head-on by working directly with clients to verify eligibility and maximize reimbursements. Our VOB process includes verifying:

VOB In Medical Billing
As your behavioral healthcare company grows and acquires more clients, you’ll be dealing with dozens of insurance companies. Longer verification hold times can disrupt your billing cycle, affecting the quality of care your employees provide to clients. If VOB is not done correctly, there is a risk that a patient may be in your care without valid benefits, resulting in no financial compensation for the facility since the billing cycle is typically a week behind.
Overall, insurance verification for incoming clients essential part of the revenue cycle management process, helping to limit surprises and ensure accurate billing, improve cash flow, and enhance the patient experience.

Thorough
Instead of using a standard or generic approach, each individual insurance policy is thoroughly verified to ensure that no claims are left unpaid or services are wrongly denied due to any inaccuracies or omissions in the policy data.
Accurate
By obtaining detailed and accurate information about each client’s specific healthcare needs, insurance companies can ensure that their clients receive the appropriate benefits and coverage they are entitled to, avoiding any denials, confusion, or frustration that may arise from inaccurate or incomplete data.
Concise
Effective communication with insurance companies is handled with expertise and precision to ensure that all necessary information is conveyed and any issues or concerns are resolved in a timely and efficient manner.

Validating
VOBs can be used for payment appeals as proof of coverage if an insurance company denies coverage for a claim, even when the services rendered are medically necessary and fall within the scope of the patient’s insurance coverage.
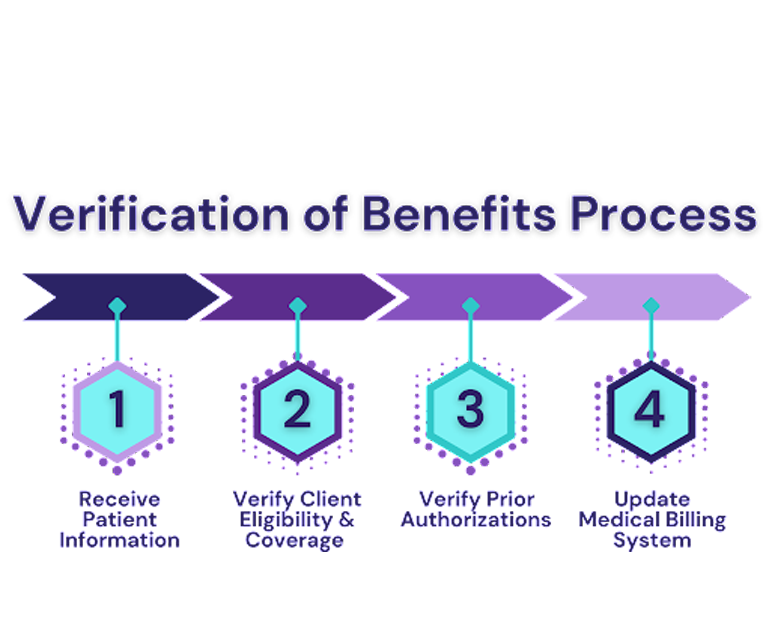
Our Verification of Benefits Process
Hansei Solutions receives patient information and schedules from addiction treatment, mental health, and dual diagnosis treatment centers to ensure efficient and timely billing processes.
We verify your patient’s insurance coverage with an eligibility check, scanning for policyholder’s details, policy effective and term dates, copay or co-insurance requirements, deductibles and out-of-pocket maximums, pre-authorization requirements, and out-of-network coverage.
Our experienced team will verify and communicate with insurance providers to ensure that any prior authorization requirements are completed accurately and efficiently.
Once insurance coverage is verified, Hansei Solutions updates the billing system with all relevant details, including the start and end dates of the client’s insurance plan, their member ID, group ID, copay information, and other critical data.

Benefits For Behavioral Healthcare Providers
VOB allows you to estimate how much your client will owe for your care, making it easier to collect payments at the time of service.
It enables you to obtain any required authorizations before delivering care or services.
VOB supports higher clean claim rates by ensuring you bill the correct insurance and use the proper billing order, even in cases where a client has more than one active policy.
Save on in-house operational costs by outsourcing to a medical billing solutions company trained in advanced VOB techniques.

Benefits For Clients
By providing clients with upfront information about the potential costs of their treatment, healthcare providers can help to reduce stress and alleviate any concerns about unexpected medical bills.
It allows clients to quickly receive estimates and copays before treatment and bills after treatment, reducing long waiting periods.
It allows clients to look for another, lower-cost provider or a different insurance policy.
It allows clients to plan for services ahead of treatment.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.