Blog

Hospitals, ambulatory surgery centers, behavioral treatment centers, and small medical practices are known for saving lives and providing healthcare. However, many of these services are owned by private companies and medical groups that also need to focus on successful business tactics, policies, and the state of their revenue cycle.
If they fall behind on submitting medical bills, following up with denied claims, and the most effective healthcare trends, their patient care quality will drop, and their business won’t last. So, how do healthcare practices stay afloat and manage their revenue cycle?
This brief article breaks down end-to-end revenue cycle management, the services usually included, and the improvements your medical practice can see in as little as a year.
What Is End-To-End Revenue Cycle Management?
End-to-end revenue cycle management (RCM) involves overseeing a medical practice’s billing and revenue process, from the initial patient appointment and information collection to the completion of treatment and all claims and payments (front-end to the back-end). This tracks patient information and bills and highlights trends and areas that need improvement. For example, a medical practice might submit claims on time with all the correct information but fail to receive prior authorization from the payer beforehand. Instead of wondering what’s wrong with your practice’s revenue, RCM provides a clear answer with reference to data and how the industry and its policies are changing.
Stages of End-To-End Revenue Cycle Management
Here’s an example of the typical stages of end-to-end revenue cycle management for an addiction treatment center.
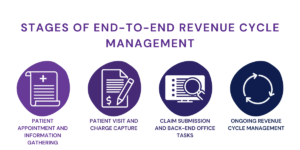
- Patient Appointment and Information Gathering: The revenue cycle begins when a patient schedules an appointment and provides information to the admissions agent, who creates a patient account.
- Patient Visit and Charge Capture: Once the patient comes into the treatment center and receives treatment, the provider or coder identifies the appropriate ICD-10 code corresponding to the treatment, determining the reimbursement amount from the patient’s health insurance.
- Claim Submission and Back-End Office Tasks: After creating a claim, it’s sent to insurance for payment. But it doesn’t stop there. Sometimes, claims are rejected due to coding errors or missing patient info. If insurance doesn’t cover everything, the practice will have to send their patient another bill for the remaining costs. This can upset patients, which is why prior authorization and benefits verification is important.
- Ongoing Revenue Cycle Management: The RCM process takes time, with claims and bills often taking months to process. Claims may bounce between payers and providers until everything is sorted out. During remittance, payers either approve and pay or deny the claim.
Read more: 5 Ways To Prevent & Appeal Medical Necessity Denials
Typical End-To-End Revenue Cycle Management Services
End-to-end revenue cycle management can be split into three steps: front-end, mid-revenue, and back-end.
Front-end services include:
- Credentialing healthcare providers and practices to ensure they’re qualified to provide specific services to patients and eligible for insurance contracts.
- Verifying patient benefits and eligibility confirms the specific services covered under a patient’s insurance plan. If a practice provides treatment to a patient without verifying their plan, the insurance will deny the claim, and the practice will have to send their patient the full bill or accept the losses due to their error.
- Prior authorization ensures that specific investigational or experimental services, such as diagnostic imaging (MRIs, CTs, and PET scans), are approved and covered by a patient’s plan. Not all services require prior authorization, but without it, payments can be denied and back up your billing process.
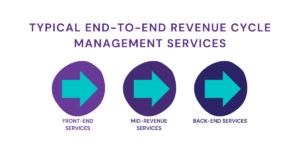
Mid-revenue services include:
- Assigning and inputting the correct treatment and procedure codes for services. This reduces the amount of payments denied because of errors or outdated codes.
- Claim management tracks the payment process and ensures payers review, process, and approve service bills.
- Payment posting helps keep track of payments from payers, allowing patients to see how much they owe after their insurance covers services and how much their services cost in the first place.
Back-end services include:
- Accounts receivable ensures that late payments from insurance companies or patients are followed up with and resolved through collection services.
- Denial management helps medical practices appeal incorrectly denied claims and correct any mistakes caught by the payer, such as incorrect codes or vague treatment timelines.
- Patient pre-collections (deductible, copays, coinsurance fees) help medical practices reduce collection costs and increase their immediate revenue.
Before You Hire A Revenue Cycle Management Company
Most of the services listed above are provided by outsourced medical billing companies, but you need to check if they just cover parts of them. For example, a smaller medical billing company might only submit claims on your behalf but won’t follow up with denied claims or missing payments. Look for a medical billing company that goes above and beyond, such as pursuing legal action for payments covered under a patient’s plan but denied because of discrimination toward the patient’s condition or disorder.
Read more: How To Find The Right Medical Billing Company In California
Benefits of End-To-End Revenue Cycle Management
End-to-end revenue cycle management (RCM) brings several advantages:
- Enhanced Efficiency: While it might seem like adding complexity, end-to-end RCM is designed to simplify the entire revenue cycle. Despite initial adjustments, the long-term return on investment (ROI) justifies the transition. It resolves redundancies, billing errors, and common challenges using advanced technology and customized management plans. This frees staff from repetitive tasks, allowing them to focus on revenue-boosting opportunities.
- Access to Expertise: Even with a sufficient workforce, the insights of industry experts can be invaluable. A reputable end-to-end RCM provider, like Hansei Solutions, comprises professionals with firsthand experience in the field. Working alongside these experts offers staff valuable on-the-job training and support for professional growth.
- Improved Collaboration: Larger healthcare organizations often suffer from departmental silos, leading to duplicated efforts and data transfer errors. Adopting a streamlined approach with end-to-end RCM can optimize the entire organization’s workflow and promote better department teamwork.
- Enhanced Communication: Engaged employees value their ability to provide feedback and address revenue issues. Integrating end-to-end RCM experts into your team provides an external perspective, creating additional touchpoints for staff to share insights and identify previously overlooked revenue opportunities.
- Access to Innovation: With the multitude of RCM technology options available, it’s challenging to determine the best investments. End-to-end RCM providers offer access to the latest revenue cycle tools and technologies validated (and sometimes created) by their experts, ensuring you stay up-to-date and efficient in managing your revenue cycle.
Contact Hansei Solutions
If you want to know more about effective end-to-end revenue cycle management solutions, contact Hansei Solutions. Our RCM team can set you up with a free demo of our revenue and billing solutions, including a preview of our latest EHR software, Benji. We offer medical billing, utilization review, denial management, contract management, and more to non-hospital healthcare facilities and behavioral treatment centers.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.