Blog

In addiction treatment and behavioral healthcare, clinical needs don’t follow rigid billing timelines. A client might need to see a psychiatrist on Monday, a trauma therapist on Wednesday, and a medical provider on Friday. Each of these sessions could be medically necessary—and potentially billable.
But this brings up a tricky question that billing teams and clinicians often face: can 2 consultations be billed in the same week?
At first glance, it seems like it should be allowed—after all, multiple evaluations may be essential to properly address the client’s needs. But payers, especially Medicare and some private insurers, see things through a more complex lens. This is where documentation, coding, and context make all the difference.
What Counts as a Consultation?
A consultation, by definition, involves one healthcare provider seeking the advice or opinion of another provider regarding a specific problem. It’s different from a routine visit or follow-up. Consultations are typically initiated by a referral and should result in a written report or summary back to the requesting provider.
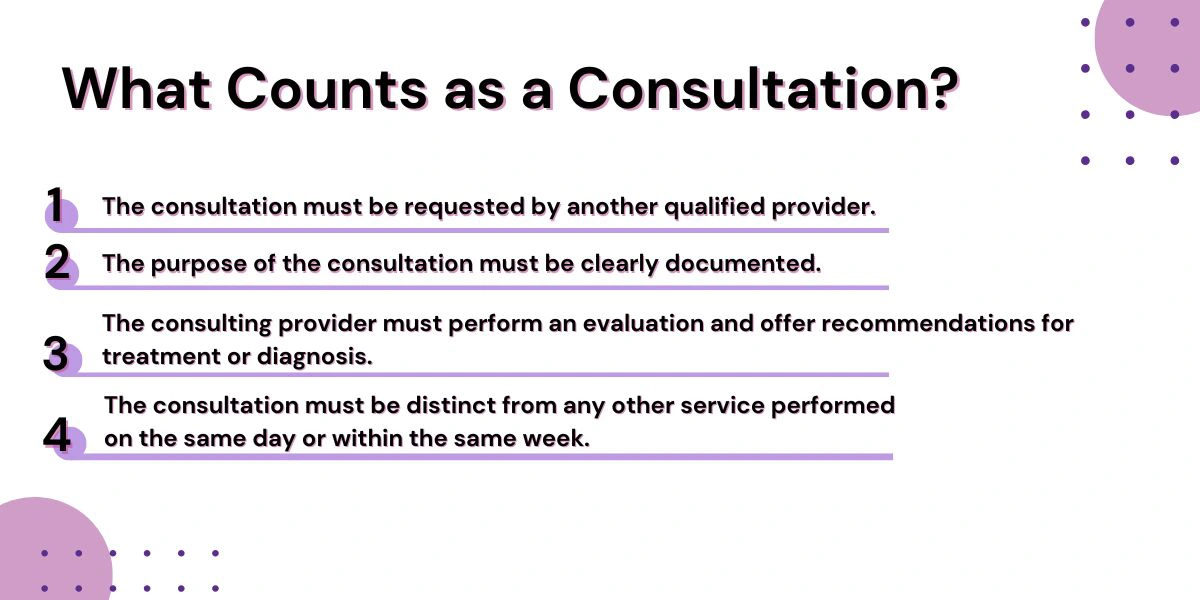
This process is structured and must meet several criteria:
- The consultation must be requested by another qualified provider.
- The purpose of the consultation must be clearly documented.
- The consulting provider must perform an evaluation and offer recommendations for treatment or diagnosis.
- The consultation must be distinct from any other service performed on the same day or within the same week.
If these criteria are met, billing for more than one consultation in a week may be appropriate. However, as noted by CMS, consultation codes (like 99242–99245 for outpatient, or 99252–99255 for inpatient) are no longer reimbursed by Medicare, requiring the use of standard evaluation and management (E/M) codes instead.
When It’s Allowed: Scenarios That Justify Two Consultations
Let’s explore when this is typically permitted:
1. Different Specialties, Separate Needs
Say a patient enters your facility and meets with a psychiatrist for mental health stabilization. Later in the week, they’re referred to an addiction medicine specialist due to signs of opioid dependency. These services can often be billed separately if each provider is from a different specialty and operates under a different taxonomy code.
2. Different Medical Conditions
Even if the same provider is involved, consultations for different conditions (say, an initial evaluation for anxiety and a later one for suspected trauma-related symptoms) may be billed separately—so long as both are clinically supported and fully documented.
3. Different Settings
If a patient is first evaluated in an outpatient office setting and later seen again during an inpatient admission, those consults might both be eligible for reimbursement. In this case, the location of care becomes an important differentiator.
4. Time-Sensitive Evaluations
In behavioral health, mental health states can change rapidly. A patient might appear stable during one evaluation but experience a severe mood or substance use crisis days later. In such time-sensitive cases, a second consultation may be appropriate and billable with the right medical justification.
Where Providers Get Into Trouble
Just because a service was rendered doesn’t mean it should be billed. Here are a few red flags that can lead to denials:
- Duplicate consultations for the same issue by the same provider without a clear change in condition.
- Vague or missing documentation, especially if there’s no documented request for consultation or if the services don’t differ in scope.
- Incorrect use of CPT codes, particularly in Medicare cases where consult codes are no longer accepted.
Payers are increasingly using artificial intelligence to detect billing anomalies. If your facility submits two consults in a week and both appear identical in code and documentation, it could trigger an audit.
For reference, guidelines from the American Medical Association and payer-specific policies should always be consulted before submitting claims involving multiple consultations.
Documentation Tips to Support Consultation Claims
Getting it right isn’t impossible—but it does require precision. Here’s what you need to document if you’re billing for two consultations in the same week:
- Clear referral source: Who requested the consultation and why? Include their full name, credentials, and reasoning in the chart.
- Detailed exam findings: Make sure the SOAP note (Subjective, Objective, Assessment, Plan) reflects the complexity of the evaluation.
- Medical necessity: Document why this consultation was essential—especially if it closely follows another.
- Distinct diagnosis or condition: If the two consults are for different issues, make that obvious in both your clinical note and coding.

Why Behavioral Health Billing Can Be More Complicated
In the field of addiction recovery and behavioral health, co-occurring disorders are the rule—not the exception. A patient may have a primary diagnosis of alcohol use disorder but also suffer from PTSD, anxiety, or major depressive disorder. Evaluating these conditions often requires insights from multiple professionals.
That’s why it’s not uncommon for different members of a clinical team—psychiatrists, psychologists, internal medicine specialists, and licensed clinical social workers—to all contribute during a patient’s first week of intake.
When billing for multiple consultations, your team must be prepared to defend the necessity and timing of each interaction. Working with a billing partner like Hansei Solutions helps ensure your documentation tells the full story—clearly, compliantly, and completely.
FAQs About Billing Consultations
Can I bill two consultations for the same patient in one week?
Yes, if each consultation is medically necessary, properly documented, and provided by a different provider or for different reasons.
Does Medicare pay for consultation codes anymore?
No. Since 2010, Medicare requires that providers use standard E/M codes instead of CPT consult codes.
Can I use the same consultation code twice in a week?
Not unless the conditions of the consults are clearly distinct. Otherwise, it can be flagged as duplicate billing.
What happens if I bill two consultations incorrectly?
At best, one of the claims will be denied. At worst, your practice could face clawbacks or be selected for an audit.
What’s the best way to ensure consultation billing is done correctly?
Work with a billing partner like Hansei Solutions, and make sure your team is trained on payer-specific rules and documentation protocols.
Let Hansei Solutions Help You Bill with Confidence
Billing multiple consultations in the same week isn’t just about codes—it’s about context. When you understand what insurers look for and how to document medical necessity, you can safely and successfully bill what you’re entitled to.
At Hansei Solutions, we specialize in guiding behavioral health and addiction treatment providers through the maze of insurance compliance. We understand the nuances, from payer policy shifts to coding updates, and we’re committed to helping you get reimbursed accurately—without the stress.
Have questions or need help with your billing process? Reach out to Hansei Solutions today and let us help you support recovery with confidence.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.