Driving Growth Through Partnership: A Revenue Cycle Success Story
Delivering 8% Net Revenue Growth in 12 Months for a Leading Multi-State Behavioral Health Organization
At Hansei, we believe that true impact comes from partnership. We work closely with behavioral health organizations to understand their unique challenges, align goals, and deliver solutions that drive sustainable growth. This commitment to collaboration made us a natural fit for this multi-state behavioral health organization that faced revenue cycle challenges.
The organization offers a full spectrum of care—from inpatient and detox to outpatient and telehealth. Collections per admission and deposit day were below expectations. Leadership needed a partner to optimize performance, strengthen utilization review, and build long term financial stability.
That’s where Hansei came in.
The Hansei Approach
During the first 18 months, Hansei streamlined operations and enhanced financial visibility by collaborating with clinical and administrative teams at the facility to improve claims accuracy and ensure payor alignment, all without disrupting patient care.

As a strategic growth partner, Hansei continued to stay committed to going beyond process improvements, actively advocating for both patients and providers. The Hansei billing team focused on holding payers accountable and protecting revenue integrity; working side by side with internal teams and payers to navigate common obstacles in revenue cycle in real time.
With payers increasingly delaying payments and requesting excessive medical records, internal revenue cycle teams often face added strain. Hansei alleviated this burden by managing the organization’s claims meticulously, ensuring timely and accurate reimbursement. This allowed facility staff to focus on what matters most: providing exceptional patient care.
The Results: Partnering for Measurable Success
All gains were achieved while the census remained stable, showing that improvements were driven by process optimization rather than growth in patient volume. Over the first 18 months of the partnership, the provider achieved measurable and sustained improvements across its revenue cycle:
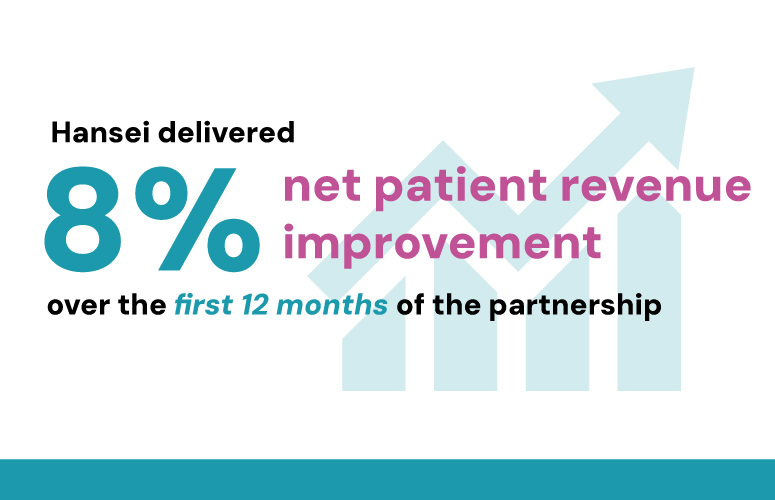
Hansei improved net patient revenue by 8% over the first 12 months of the partnership.
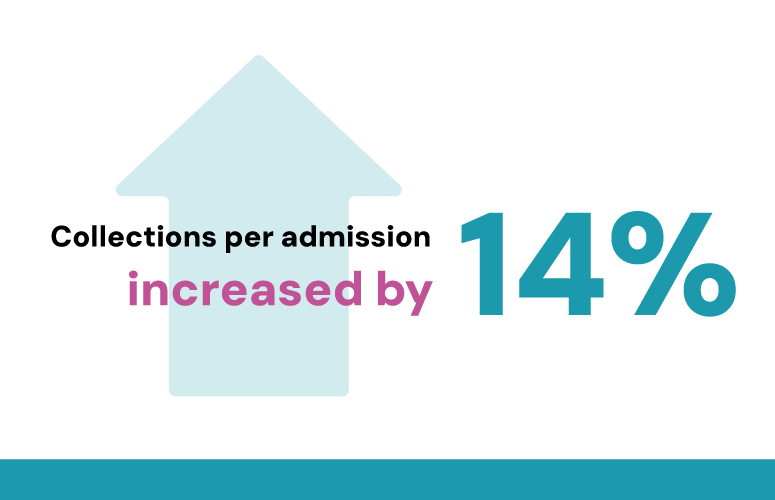
Revenue collected per patient admission increased by 14%.
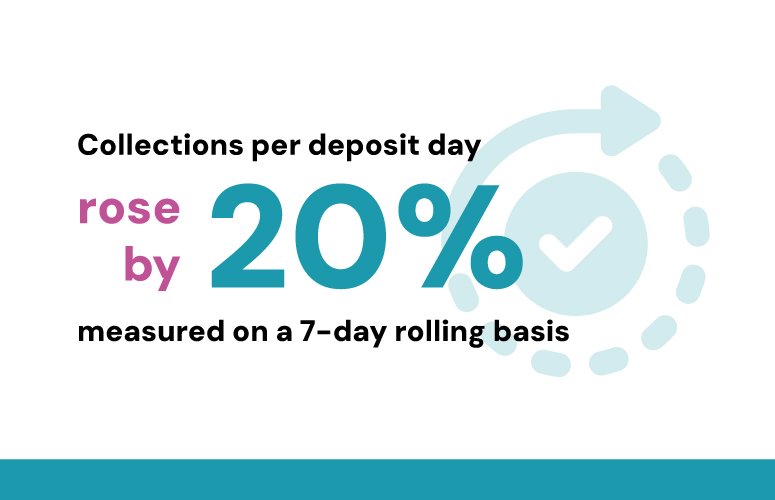
Collections per deposit day rose by 20% when measured on a 7-day rolling basis — reflecting stronger, more consistent cash flow and sustained improvement in collection efficiency over time.
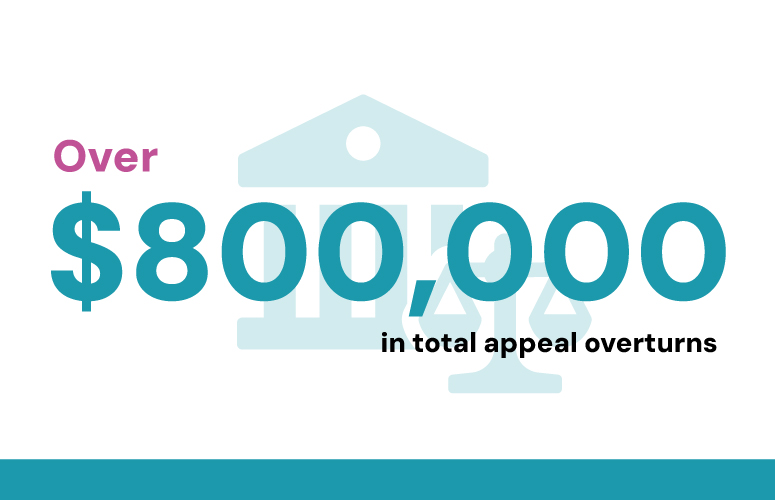
Successfully overturned over $800,000 in denied claims.
Addressed and resolved Medicaid-related payment issues exceeding $500,000.

Resolved outstanding claims with a Union Third Party Administrator, totaling over $340,000.

Tricare Claims Consistent
Escalated and prioritized Tricare relationship for steady claims processing and payments.
This partnership shows how a committed facility team focused on delivering excellent care leveraged the Hansei strategic partnership to strengthen financial results. The organization was able to achieve sustainable growth and reinvest in what matters most — its patients. At
Hansei we understand organizational dedication to patient care and we are grateful to parter with facilities of all sizes to further their mission and access to treatment.