Blog
The healthcare revenue cycle management process is the backbone of financial stability for behavioral health centers. From the moment a patient schedules an appointment to the time the final payment is collected, every step in the cycle matters. In behavioral health, where services often involve recurring sessions, complex payer rules, and detailed documentation, effective revenue cycle management (RCM) can mean the difference between financial success and constant strain.
At Hansei Solutions, we help behavioral health centers streamline the RCM process, reduce denials, and free up providers to focus on delivering exceptional patient care.
What Is the Healthcare Revenue Cycle Management Process?
The healthcare revenue cycle management process refers to the system providers use to track, manage, and collect payment for patient services. It covers everything from insurance verification to final collections. In behavioral health, the process is especially critical because payer requirements and billing codes are often more complicated than in other areas of healthcare.
According to the Centers for Medicare & Medicaid Services (CMS), behavioral health providers must meet specific criteria and maintain detailed documentation for services to be considered reimbursable. Without a strong RCM strategy, providers risk high denial rates and delayed payments.
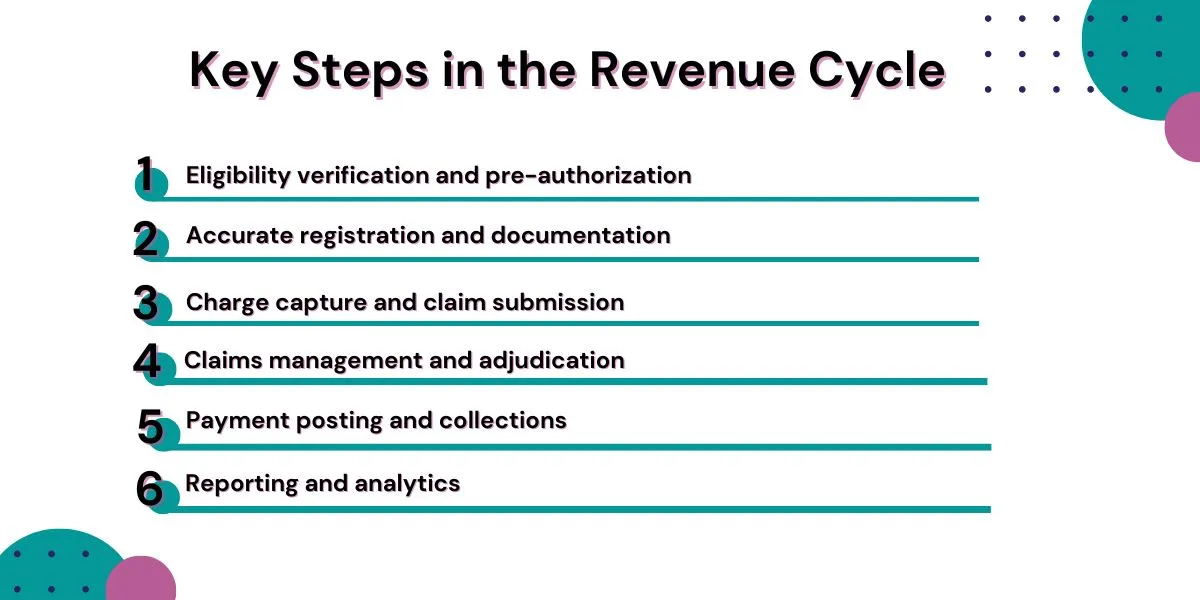
Key Steps in the Revenue Cycle
While workflows may vary across organizations, most behavioral health centers follow a similar sequence:
- Eligibility verification and pre-authorization – Confirming patient coverage before treatment begins.
- Accurate registration and documentation – Recording demographic details, clinical notes, and payer-required information.
- Charge capture and claim submission – Coding services correctly and submitting claims promptly.
- Claims management and adjudication – Addressing payer reviews, denials, or requests for more information.
- Payment posting and collections – Recording payments and following up on outstanding balances.
- Reporting and analytics – Reviewing denial trends and aging reports to improve financial performance.
Each step has unique challenges in behavioral health. For example, SAMHSA notes that even screening and brief intervention services require specific coding to ensure reimbursement.

Why Revenue Cycle Management Matters in Behavioral Health
Behavioral health centers face challenges that general healthcare providers often do not. Payers frequently demand extra documentation to justify therapy sessions or substance use treatment. Pre-authorization requirements can delay timely access to care. And billing multiple sessions per week creates more opportunities for errors.
Strong revenue cycle management ensures:
- Patients receive care without unnecessary delays.
- Providers are reimbursed fairly and quickly.
- Centers maintain the financial stability needed to expand services.
Common Challenges for Behavioral Health Providers
Even well-run behavioral health centers encounter obstacles in the RCM process:
- High denial rates caused by coding errors or insufficient documentation.
- Prior authorization delays that slow treatment access.
- Inconsistent payer requirements that vary across insurance plans.
- Patient billing challenges as out-of-pocket costs rise.
Reports have found that insurance reimbursement for behavioral health services is often inconsistent, creating additional stress for providers and patients.
How Hansei Solutions Supports Behavioral Health Centers
At Hansei Solutions, we take the guesswork out of revenue cycle management. Our team provides:
- Hands-on support with eligibility checks and pre-authorization.
- Streamlined claims submissions to reduce administrative burdens.
- Ongoing monitoring of denials with rapid resolution strategies.
- Patient-friendly billing communication that encourages timely payments.
- Comprehensive reporting that identifies long-term opportunities for improvement.
By managing these tasks, we help behavioral health centers optimize their healthcare revenue cycle management process while keeping the focus where it belongs—on patient outcomes.
FAQs About Healthcare Revenue Cycle Management
Why is RCM especially important for behavioral health centers?
Because these centers face payer rules and documentation requirements that are stricter than most other specialties, making reimbursement harder to secure.
What are the biggest RCM challenges for behavioral health providers?
Frequent denials, complex pre-authorizations, and inconsistent payer policies.
How does RCM improve patient care?
By reducing billing delays and administrative burdens, providers can focus more on treatment and less on paperwork.
Can outsourcing RCM help behavioral health centers?
Yes. Partnering with experts like Hansei Solutions reduces denials, improves collections, and creates financial stability.
Building a Healthier Financial Future
The healthcare revenue cycle management process is vital to the sustainability of behavioral health centers. From eligibility verification to claims resolution, each step plays a role in ensuring providers are paid and patients receive uninterrupted care. Hansei Solutions works alongside behavioral health providers to simplify this process, strengthen payer relationships, and improve financial performance—ultimately benefiting both patients and organizations.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.