Blog

Table of Contents
Clean claims indicate your medical practice follows proper medical billing, coding, and processing guidelines. But if your practice isn’t tracking clean claims or taking steps to main their consistency, your cash flow and reputation with payers can quickly deteriorate.
What Are Clean Claims?
A clean claim is a submitted claim for payment that doesn’t have any mistakes or problems. These mistakes can include missing information that slows down the payment process or leads to denials. To make a claim clean, certain important details need to be there, and if they’re missing, hard to read, or wrong, the payment request can be denied or rejected.
Here are the requirements qualifying a submitted claim as clean: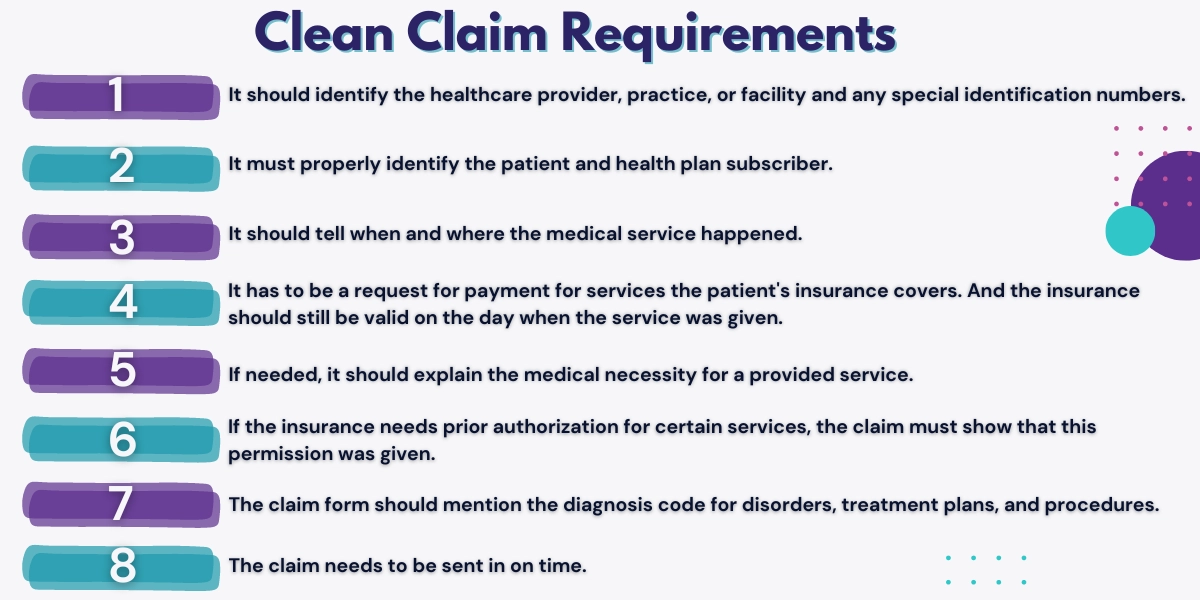
- It should identify the healthcare provider, practice, or facility and any special identification numbers.
- It must properly identify the patient and health plan subscriber.
- It should tell when and where the medical service happened.
- It has to be a request for payment for services the patient’s insurance covers. And the insurance should still be valid on the day when the service was given.
- If needed, it should explain the medical necessity for a provided service.
- If the insurance needs prior authorization for certain services, the claim must show that this permission was given.
- The claim form should mention the diagnosis code for disorders, treatment plans, and procedures.
- The claim needs to be sent in on time.
Read more: Revenue Leakage In Healthcare: Sources & Solutions
How Are Clean Claims Calculated?
The clean claim rate is calculated when an insurance claim gets paid and sorted correctly on its first try. To calculate your practice’s clean claim rate, use this formula recommended by the Healthcare Financial Management Association (HFMA):
- Divide the number of claims that pass all checks without needing manual help by the total number of claims accepted into the billing system.
What Are “Dirty” Claims?
A dirty claim is submitted to a payer with errors, requires manual processing to resolve mistakes, or is rejected. A claim that isn’t paid the first time can eat into your practice’s time and money. If your claims aren’t accepted and begin to back up, your practice could be at risk of shutting down when you’re unable to pay office rent, employees, and other bills. The Medical Group Management Association (MGMA) says fixing a rejected claim costs about $25 for each claim. If your practice has around 100 claim denials every month that need fixing, it costs about $2,500 each month. That’s about $30,000 a year for your medical practice.
Can You Increase Your Practice’s Clean Claims?
Yes, you can increase your practice’s amount of clean claims, also called a clean claim rate. Most experts agree that an acceptable clean claim rate is around 80%, but to ensure quality, accuracy, and good relationships with payers, you should aim for 90% or higher.
Make sure your patient information is correct: Small mistakes in patient information can easily lead to a claim being rejected. To avoid these errors, ensure patient details are updated in the electronic health record (EHR), updating information during each follow-up appointment.
Stay updated on medical billing and coding regulations: Rules for medical coding are always changing. Even if you have staff in your office who handle medical billing, staying updated with the latest changes can be hard. Outsourcing your medical billing can take the weight off your staff’s shoulders and allow them to focus on patients rather than bills.
Perform daily and weekly quality checks and audits: Quality assurance plays a crucial role before submitting claims. Ensure the appropriate amount of billable hours are accounted for, signatures from clinicians or supervisors are provided, and state and national guidelines are followed.
Read more: Healthcare Patient Retention: Importance, Strategies, & Calculation
How To Maintain Clean Claims
Claim scrubbing: Claims scrubbing is the process of checking claims before submitting them to insurers to ensure they’re accurate, complete, and have the correct codes. This increases the chances the insurer pays each claim quickly. If any information in the claim doesn’t match the rules or seems incorrect, the software flags it as an error or an inconsistency. These errors include missing patient information, incorrect codes, or mismatched data.
Medical billing partner: Partnering with a medical billing partner who can follow up and appeal denied claims is a great way to maintain a consistent, clean claim rate. These dedicated teams will monitor claim submissions, see where errors result, and implement changes to correct mistakes. They can also work with and educate your medical staff to ensure that the initial code input process is seamless and claims are processed correctly from the beginning.
Medical billing software: Another significant factor in maintaining a high clean claim rate is using powerful healthcare billing software in your practice, such as Benji. Many services offer billing analytics tools to assist with prior authorizations and identify code errors when they are posted, but not all of them help with customer relationship management (CRM) or revenue cycle management (RCM). These software components set new medical practices apart from educated and experienced practices with integrative billing solutions.
Contact Hansei Solutions
If you want to increase your medical practice’s clean claim rate, contact Hansei Solutions. Our medical billing and RCM teams are dedicated to helping reduce billing errors that could cost your medical practice tens of thousands of dollars in revenue. We offer medical billing, utilization review, denial management, verification of benefits, and more! Call today, and one of our billing specialists can set you up with a free demonstration of our solutions and software.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.