Blog

Let’s face it—billing for behavioral health services can be a real headache. Between juggling insurance rules, handling endless codes, and making sure everything gets submitted correctly, it’s no wonder so many providers feel overwhelmed. But don’t worry—this guide breaks down everything you need to know about billing for behavioral health services. Whether you’re just starting out or looking for ways to make the process smoother, you’re in the right place.
Why Is Behavioral Health Billing Unique?
Billing for behavioral health isn’t the same as billing for other medical services. The services themselves—like therapy sessions, psychiatric evaluations, and group counseling—are different. And because of this, insurance companies handle them differently too. You’ll need to consider things like time-based codes (think 90837 for a 60-minute therapy session), prior authorizations, and coverage limits.
Behavioral health services also often require the use of unique modifiers that provide additional details about the services rendered. Insurance companies may have specific rules about how and when these modifiers should be applied, and not following them can result in denied claims. Another layer of complexity comes from the constantly evolving healthcare regulations that behavioral health providers must stay on top of to remain compliant. Add in the emotional and personal nature of the services provided, and it’s clear why billing for behavioral health is uniquely challenging.
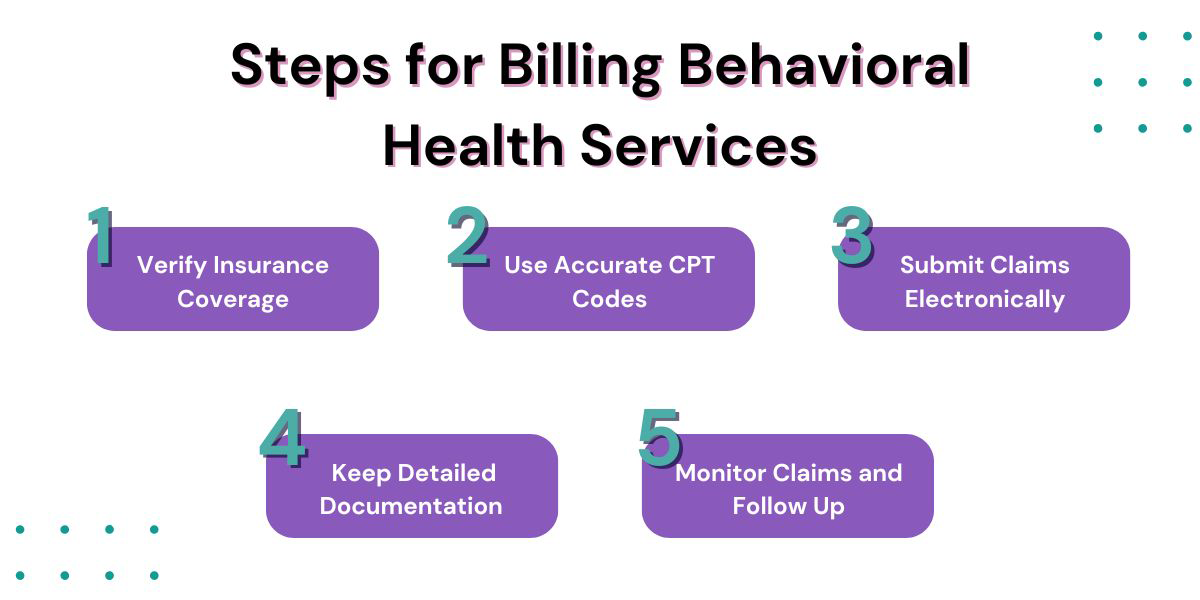
Steps for Billing Behavioral Health Services
Getting paid for behavioral health services isn’t just about sending an invoice. It’s a multi-step process that takes some careful attention. From checking insurance to keeping track of claims, each step is critical. If you follow these steps, you’ll not only avoid common pitfalls but also keep your revenue flowing steadily.
1. Verify Insurance Coverage
Before you even start, make sure you understand what the patient’s insurance will cover. Are their therapy sessions included? What about co-pays and deductibles? Do you need prior authorization? Verifying this upfront can save you from surprises later on, like denied claims or unexpected out-of-pocket costs for the patient. Don’t forget to document everything during this process, as it can serve as a reference if issues arise later.
2. Use Accurate CPT Codes
CPT codes are the language of billing, so getting them right is non-negotiable. For instance, 90791 is for an initial psychiatric evaluation, while 90834 is for a 45-minute therapy session. Mistakes here can lead to claim denials or underpayment.
To ensure accuracy, it’s important to regularly review coding updates, as the healthcare industry frequently revises these codes. Misusing codes not only slows down reimbursement but can also put your practice at risk of audits. Consider investing in coding resources or training for your staff to minimize errors.
3. Submit Claims Electronically
Filing claims electronically isn’t just quicker—it’s also more accurate. Most insurance companies prefer this method, and it makes tracking claims much easier. Plus, you’ll get feedback faster, so you can fix any issues before they become major problems. An electronic submission system often includes built-in error checks to catch mistakes before the claim is even sent, saving time and effort.
4. Keep Detailed Documentation
Good documentation isn’t just a best practice—it’s a must. Make sure your notes include the session’s date and time, the patient’s progress, and any specific interventions you used. This level of detail isn’t just about getting paid—it’s also crucial for compliance and continuity of care. For instance, clear documentation can make it easier to justify the necessity of services if an insurance company requests additional information.
5. Monitor Claims and Follow Up
Once your claims are submitted, don’t just sit back and wait. Keep an eye on their status and be ready to follow up on any denials or delays. The sooner you address issues, the faster you’ll get paid. Monitoring claims closely can also help identify patterns, like recurring issues with specific insurance companies or coding errors that need to be addressed.
Common Challenges in Behavioral Health Billing
Billing for behavioral health services isn’t without its hurdles. Denied claims are one of the biggest headaches, often caused by incomplete information or incorrect coding. Then there are the insurance limitations—some plans restrict the number of covered sessions or require pre-approvals.
On top of these challenges, managing patient expectations can add another layer of complexity. Many patients may not fully understand their insurance coverage, leading to confusion about out-of-pocket costs. This makes it even more important for providers to clearly communicate financial policies and insurance details upfront. Staying on top of frequently changing healthcare regulations is yet another challenge, requiring ongoing education and adaptation.
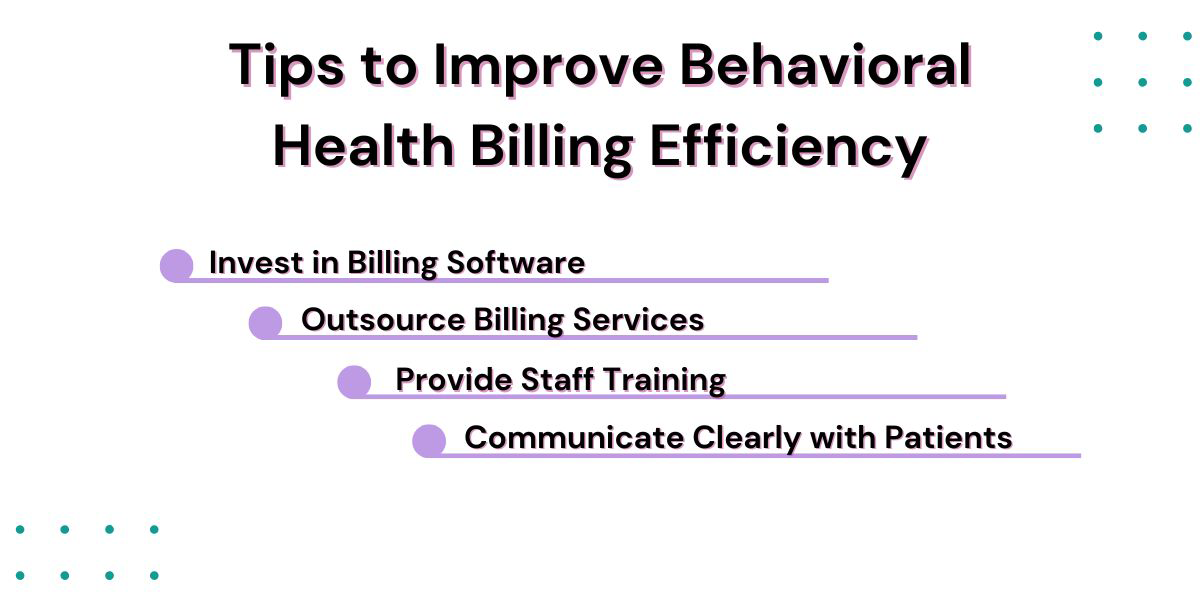
Tips to Improve Behavioral Health Billing Efficiency
Looking to make billing a little less stressful? Here are a few tips that can help:
- Invest in Billing Software: Automated systems can streamline the process, reduce errors, and make tracking claims easier.
- Outsource Billing Services: Working with a professional billing company ensures compliance and maximizes reimbursements, allowing you to focus on patient care.
- Provide Staff Training: Regularly updating your team on the latest coding rules and insurance policies can prevent mistakes and delays.
- Communicate Clearly with Patients: Setting clear expectations about costs and coverage can build trust and reduce confusion. Educating patients about their benefits can go a long way in preventing misunderstandings.
Let Hansei Solutions Simplify Your Billing Process
At Hansei Solutions, we know how challenging behavioral health billing can be. That’s why we specialize in helping treatment centers just like yours. From ensuring compliance to reducing claim denials, we’re here to make your billing process as smooth as possible.
We offer tailored solutions designed specifically for behavioral health providers, so you can rest easy knowing your billing is in expert hands. With our team handling the details, you can focus on what you do best—providing exceptional care to your patients.
If you’re ready to simplify your billing process and maximize your reimbursements, reach out to us today. Let’s navigate the complexities of billing together and set your practice up for success.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.