Blog

Billing insurance for massage therapy can feel overwhelming, especially if you’re just starting to navigate this process. But with a clear roadmap, understanding essential steps, and knowing the common pitfalls to avoid, you can make insurance billing a smooth and rewarding part of your practice.
Is Massage Therapy Covered by Insurance?
The first step to billing insurance for massage therapy is determining whether your client’s insurance policy covers massage treatments. Unfortunately, coverage can vary significantly between insurance providers and individual policies. According to a study published by the International Journal of Therapeutic Massage and Bodywork, around 27% of insurance plans explicitly exclude massage therapists from their covered providers.
However, don’t get discouraged—many plans do cover massage therapy when deemed medically necessary. For instance, massage is often covered when part of a comprehensive treatment plan, especially when prescribed by a physician or chiropractor.
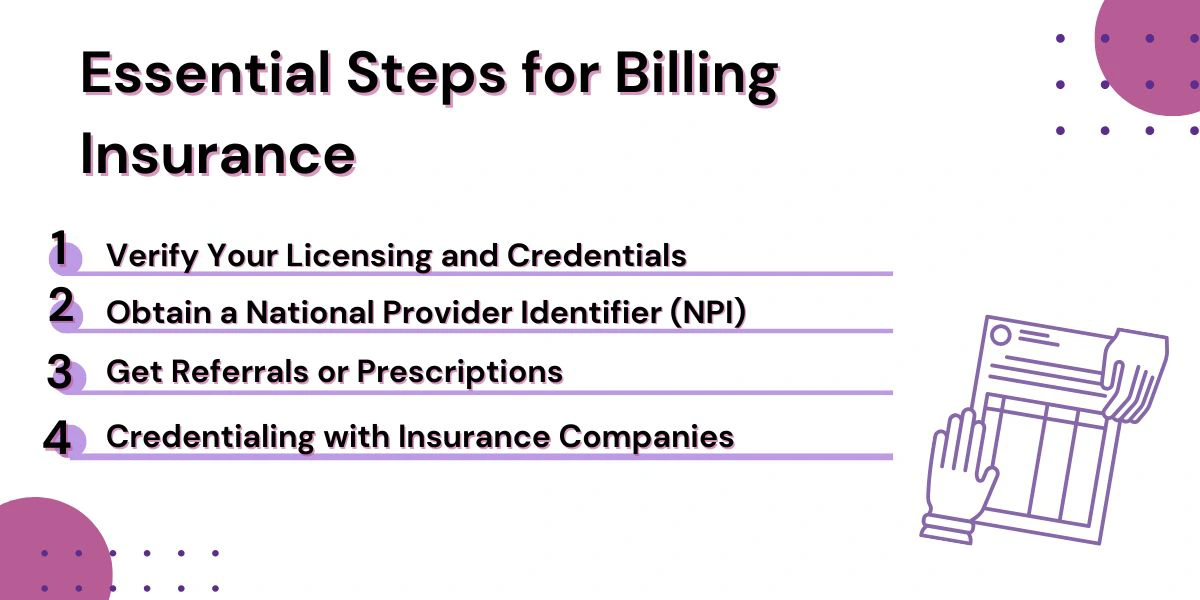
Essential Steps for Billing Insurance
Billing insurance for massage therapy involves more than just submitting a claim—it requires a thorough understanding of medical coding, coverage verification, documentation, and insurer protocols. Whether you’re new to the process or looking to refine your current system, following a clear set of essential steps can improve your chances of reimbursement and reduce claim denials. Let’s break down the key actions massage therapists should take to ensure a smooth and compliant insurance billing process.
1. Verify Your Licensing and Credentials
Before you bill insurance, make sure you meet your state’s specific licensing requirements for massage therapy. Each state has different rules about what qualifies you to bill insurance, so check with your local board or regulatory agency.
2. Obtain a National Provider Identifier (NPI)
An NPI is like your healthcare provider ID card. You’ll need one to bill insurance companies efficiently. You can easily apply for an NPI number online through the National Plan and Provider Enumeration System (NPPES)—and it’s free!
3. Get Referrals or Prescriptions
Insurance companies typically require a medical professional’s referral or prescription to validate the necessity of massage therapy. According to the American Massage Therapy Association (AMTA), approximately 67% of clients have had massage therapy recommended by their primary care doctor. This step helps ensure your claims won’t get denied.
4. Credentialing with Insurance Companies
Credentialing is the formal process of becoming an approved provider with insurance companies. Although it can take several months, once you’re credentialed, your billing process becomes much easier. Each insurance company will have specific documentation required, so start by contacting their provider enrollment departments directly.
Understanding CPT Codes
To bill insurance, you’ll need to use Current Procedural Terminology (CPT) codes, which standardize medical procedures and treatments. Some of the most common CPT codes for massage therapy include:
- 97124 – Massage Therapy: This code covers common massage techniques like effleurage, petrissage, and tapotement. It’s typically billed in 15-minute increments.
- 97140 – Manual Therapy: This includes joint mobilization, manual traction, and lymphatic drainage, also billed per 15 minutes.
- 97010 – Hot/Cold Packs: Application of moist heat or cryotherapy can be billed with this code.
Remember, insurance companies have guidelines on how these codes should be used. For example, CPT codes 97124 and 97140 are typically not reimbursed when billed together for the same session.
Best Practices for Successful Insurance Billing
Let’s be honest—billing insurance for massage therapy can feel like learning a whole new language. Even after you’ve got the basics down, staying on top of what actually leads to successful claims (and gets you paid) is a different challenge altogether. That’s where a few smart habits and insider tips can make all the difference.
Always Verify Patient Eligibility
One common mistake is not confirming coverage beforehand. Always check with the insurance provider to confirm eligibility for massage therapy services. This helps prevent denied claims and ensures clarity for your client (Holistic Billing Services).
Maintain Thorough Documentation
Good documentation is your strongest ally in insurance billing. Use detailed SOAP (Subjective, Objective, Assessment, Plan) notes for every session. These notes justify your treatments and become invaluable if you need to appeal a denied claim (MassageBook).
Stay Updated on Insurance Regulations
Insurance rules can frequently change, and staying informed is crucial. Be proactive by periodically checking your insurer’s policies and guidelines. Policies can differ significantly depending on the state, provider, or even the year (Healthie).
Navigating Challenges and Advocacy
Despite growing recognition of massage therapy benefits, insurance billing still presents challenges. As mentioned earlier, some policies explicitly exclude massage therapy coverage. Advocacy remains crucial to improving coverage and recognition for massage therapists.
The Affordable Care Act does include provisions intended to prevent discriminatory coverage practices, but consistent enforcement remains a challenge. Active participation in professional organizations, like the AMTA, can amplify therapists’ voices in healthcare policy conversations.
Common Reasons Claims Get Denied (and How to Avoid Them)
Insurance claims for massage therapy often get denied for avoidable reasons:
- Incomplete Documentation: Ensure all paperwork is complete and accurate.
- Incorrect CPT Codes: Use appropriate and specific codes for the services rendered.
- Missing Referrals: Always obtain and document referrals or prescriptions when required.
- Exceeding Allowed Visits: Track the number of covered sessions allowed under a patient’s plan.
By paying attention to these details, you can significantly decrease the likelihood of denials.
Getting the Most Out of Insurance Billing for Massage Therapy Services
Insurance billing for massage therapy can be complicated, but with the right approach, it doesn’t have to be a constant source of stress. By verifying benefits upfront, using proper billing codes, keeping thorough documentation, and understanding what insurers require, you can improve your chances of timely and full reimbursement. These efforts not only support the financial health of your practice but also make your services more accessible to clients who depend on insurance coverage.
If you’re ready to simplify your billing process and get the most out of every claim, Hansei Solutions is here to support you. Our experienced team specializes in handling the details so you can focus more on your clients and less on paperwork. Reach out today to see how we can help your practice thrive.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.