Blog

Upcoding is a serious and fraudulent practice that can cost healthcare providers their licenses, practices, and relationships with patients, payers, and communities. While upcoding isn’t something done by respectable medical providers, it’s still prevalent in the healthcare marketplace and deserves some spotlight.
This article explains what upcoding is, what unbundling is, why doctors, hospitals, and medical billing companies might upcode, and how this impacts your practice and patients.
What Is Upcoding In Healthcare?
Upcoding is when a healthcare provider submits a CPT code to private insurers or government programs like Medicare or Medicaid for a more serious and usually more expensive diagnosis or procedure than actually provided to their patient. This is fraud and a violation of the federal False Claims Act, which also allows private citizens to sue healthcare providers caught upcoding.

Medical practices and hospitals must use Current Procedural Terminology (CPT) codes for tests, procedures, and diagnoses. Insurance providers and other payers use these codes to determine how much the service costs and how much they’ll cover based on their insured’s plan. If a patient is paying out-of-pocket, the upcoded service will fall on them to pay. Upcoding directly impacts consumers and the economy since healthcare programs like Medicare are funded by taxpayers.
Read more: The Negative Effects Of Medical Billing Discrepancies On Your Practice
What is Unbundling?
Unbundling or “fragmentation” is another form of defrauding insurance providers and government programs. Programs like Medicare and Medicaid have payment packages that bundle procedures commonly performed together with lower reimbursement rates. For example, performing a needle insertion as a standalone procedure requires a specific code. However, if it’s part of a more complex procedure, providers will use a CPT code for the entire procedure.
For diagnostic nasal endoscopies, if a nosebleed is cauterized during the procedure, providers use the CPT code for the endoscopy without adding a separate code for cauterization. However, if cauterization happens separately on the same day, providers are required to add a modifier to indicate it’s a distinct service.
Unbundling and submitting these procedures separately is meant to increase a provider’s profits. Some medical providers might restrict their electronic health records to show only CPT codes with higher reimbursement rates or copy and paste patient notes from different visits to appear as if they diagnosed and treated every condition listed.
Why Would Doctors Upcode?
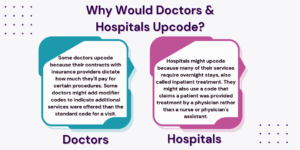
Some doctors upcode because their contracts with insurance providers dictate how much they’ll pay for certain procedures. If a medical practice is known for frequently providing a typically inexpensive procedure, they might use upcoding to increase their profits and bypass the payer contract, without actually providing a new service. Some doctors might add modifier codes to indicate additional services were offered than the standard code for a patient visit.
This can happen in specialty practices, such as psychologists using codes that reflect longer therapy session times, or psychiatrists might use CPT codes that represent more expensive or name-brand medications rather than generic ones.
Upcoding might be happening without the medical staff even knowing, with administrators upcoding services to boost their profits and professional standing within the healthcare community.
Read more: 5 Ways To Prevent & Appeal Medical Necessity Denials
Why Would Hospitals Upcode?
Hospitals might upcode because many of their services require overnight stays, also called inpatient treatment. Inpatient costs are paid using pre-determined rates according to their diagnosis-related group (DRG). However, some hospitals will use a higher level of care code even though their patient’s diagnoses are less severe or extensive. They might also use a code that claims a patient was provided treatment by a physician rather than a nurse or physician’s assistant, which are less expensive services.
As hospital care is typically more costly than standard primary practice treatment, upcoding can result in expenses ranging from thousands to hundreds of thousands of dollars for both payers and patients. The Office of Inspector General (OIG) found that from 2014 to 2019, hospital bills for the highest level of inpatient care increased by 20%. Another report found that hospital bills for the highest level of inpatient care in 2019 accounted for 40% of all cases billed to Medicare, totaling $54.6 billion. The OIG also found that 30% of inpatient stays at hospitals were unusually short and for less severe cases that didn’t require these stays.
Other practices that might upcode include:
- Medical billing companies might upcode because they want to improve their client’s profits and appear more effective and useful.
- Urgent care facilities might upcode to increase profits if they don’t frequently see many patients.
- Medical equipment providers might upcode for more expensive equipment than provided.
How This Impacts Your Practice & Patients
Upcoding is illegal, and if healthcare providers are convicted, they risk losing their license, practice, and serve jail time. One California doctor in 2019 was sentenced to prison for almost eight years for upcoding false claims of approximately $12 million to Medicare and profited almost $4.5 million. Since 2007, the Medicare Fraud Task Force has charged more than 4,200 defendants who collectively billed Medicare programs for nearly $19 billion.
Upcoding also affects the financial and physical health of patients. Insurance providers and government programs will be less likely to approve claims for higher levels of medical care if they’re overloaded with fraudulent cases since they distribute the cost of healthcare among all their carriers. Additionally, incorrect patient medical records can impact a patient’s care in the future and cause them to receive unnecessary treatments. This impacts their wallets and trust in the healthcare system.
Contact Hansei Solutions
Upcoding is a serious situation, and Hansei Solutions takes proactive measures to ensure our clients coding and billing process is accurate, efficient, and following payer, state, and national guidelines. Whether you’ve recently opened your practice or want to improve your medical billing and coding process, Hansei Solutions will guide you through every standard and advanced challenge. We’ll also help you establish better contracts with payers to ensure your services are recognized and receive the reimbursement you deserve.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.