Blog

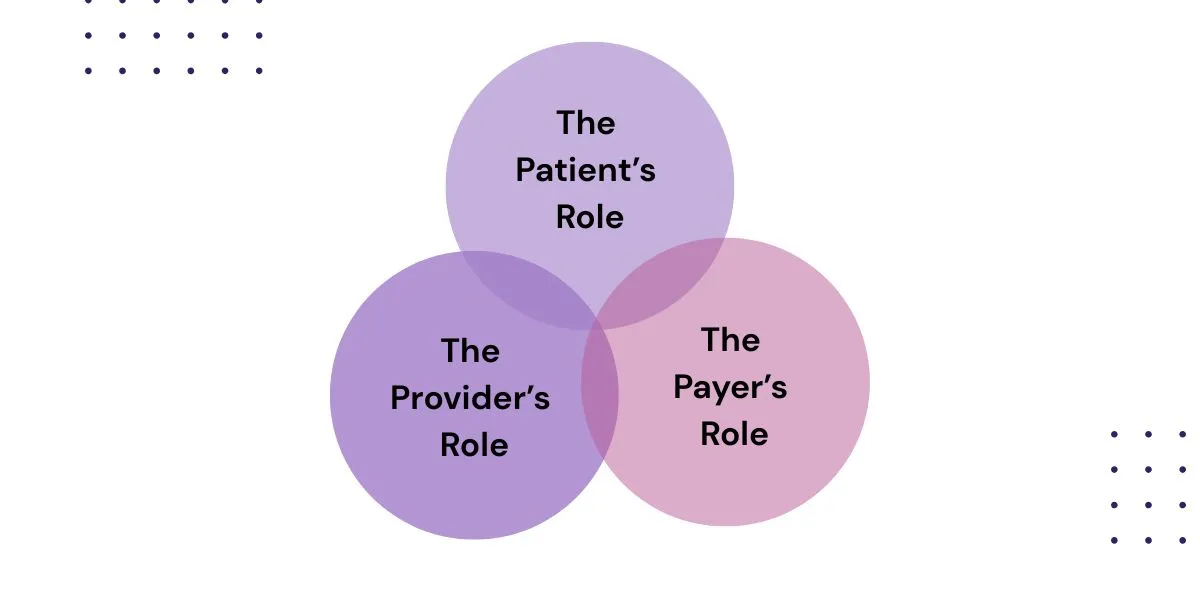
In the healthcare industry, the patient, provider, and payer relationship forms the foundation of how care is delivered, financed, and experienced. This three-way dynamic determines not only the quality of patient outcomes but also the efficiency and financial sustainability of healthcare organizations. At Hansei Solutions, we believe understanding this relationship is essential to improving both patient experiences and provider operations.
What is the Patient, Provider, and Payer Relationship?
At its core, the patient, provider, and payer relationship describes the interaction between three key players. Patients are the individuals seeking medical services and support. Providers are the professionals and organizations delivering care. Payers, such as insurance companies, government programs, or self-funded employers, finance the costs. Together, these groups create a cycle: patients need care, providers deliver it, and payers reimburse or cover expenses.
When these groups are in sync, healthcare runs smoothly. When they are not, patients may face delays or unexpected bills, providers may struggle with administrative challenges, and payers may see rising costs.
Why This Relationship Matters
Each group has its own priorities. Patients want accessible and affordable care. Providers depend on timely, fair reimbursement to keep their practices running. Payers are focused on controlling costs while ensuring members receive effective treatment.
When these goals overlap, outcomes improve. Strong collaboration helps patients get the care they need, supports providers in focusing on treatment instead of paperwork, and allows payers to manage resources responsibly. However, misalignment—like denied claims or complicated billing—can strain the entire system.
The Patient’s Role
Patients sit at the center of this relationship. Their responsibilities include choosing providers within their network, sharing accurate health information, and working with providers on treatment plans. They are also responsible for understanding their coverage details, such as deductibles or co-pays. Ultimately, patients benefit most when providers and payers remove barriers to care, whether that means cutting down on prior authorizations or simplifying billing.
The Provider’s Role
Providers act as the bridge between patients and payers. They deliver high-quality care, document medical necessity, and submit claims for reimbursement. At the same time, they must help patients navigate financial responsibilities and treatment options.
Unfortunately, administrative tasks like denied claims or excessive paperwork often pull providers away from what they do best—caring for patients. This is why Hansei Solutions works closely with healthcare organizations to streamline revenue cycle management and allow providers to dedicate more energy to treatment.
The Payer’s Role
Payers play a powerful role in this relationship. They set policies for covered services, review claims, and determine reimbursement. While payers aim to manage costs, their decisions also directly affect how quickly patients access care and how smoothly providers get paid.
Clear and timely communication with both patients and providers is essential to avoid disputes or delays. When done right, payers can encourage cost-effective, high-quality care that benefits everyone.
Common Challenges in the Relationship
Even though this three-way connection is crucial, it is not without challenges. Claim denials, coverage gaps, and administrative complexity can create unnecessary delays. Patients may feel frustrated when faced with unclear billing or surprise costs. Providers may struggle when reimbursements are delayed or denied. And payers may find themselves balancing financial sustainability with ensuring proper access to care.
At Hansei Solutions, we focus on reducing these friction points, helping providers cut down on denied claims and making the financial side of healthcare less burdensome for all parties involved.
How Hansei Solutions Strengthens the Relationship
Hansei Solutions improves the patient, provider, and payer relationship by aligning the goals of all three groups. We help providers reduce administrative headaches and accelerate reimbursement, while also promoting transparency so patients better understand their financial responsibilities. Our team works to build collaborative partnerships with payers, transforming the process from conflict-driven to solution-oriented.
By streamlining these connections, we create healthier, more sustainable systems where providers thrive financially, patients feel supported, and payers achieve better resource management.
FAQs About the Patient, Provider, and Payer Relationship
Why is this relationship so important in healthcare?
Because it influences whether patients receive timely, affordable care while ensuring providers are fairly compensated and payers can control costs.
What are common issues that disrupt this relationship?
Some of the most frequent challenges include claim denials, prior authorization delays, and coverage confusion.
How can providers strengthen their relationship with payers?
By maintaining accurate documentation, staying compliant with payer policies, and working with revenue cycle partners like Hansei Solutions to streamline claims.
How does this relationship affect patients directly?
Patients may face delays or unexpected costs if providers and payers are not aligned. Strong communication leads to smoother care and billing.
What role does Hansei Solutions play in this relationship?
We simplify revenue cycle management, reduce denied claims, and strengthen provider-payer communication, ultimately improving the patient experience.
Keeping Peace in Patient, Provider, and Payer Relationships
The patient, provider, and payer relationship is the cornerstone of a functional healthcare system. When all three parties collaborate effectively, patients receive better care, providers can focus on treatment instead of administrative tasks, and payers manage costs sustainably. Hansei Solutions is here to strengthen these connections, ensuring healthcare works better for everyone.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.