Blog

Table of Contents
A denial claim is when a health insurance company or payer denies paying for services requested by an individual or healthcare provider. These claims represent lost revenue (when the claim is not paid even after appeals) or delayed revenue (when the claims are paid after appeals).
Healthcare organizations should be concerned about denied claims since they can hold back their company’s growth. When a healthcare provider encounters a denied claim, the biller needs to conduct a root-cause analysis to identify and correct the underlying issues before filing an appeal with the payer.
In this article, we will cover the types of claim denials, the steps to prevent claim denials, how to mitigate your losses, and some solutions to claim denials.
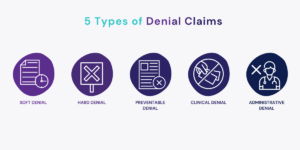
Types Of Claim Denials
Primarily, claim denials fall under five categories: –
- Soft Denial – Soft denial is a temporary denial that can be resolved by taking the correct actions without needing an appeal.
- Hard Denial – Hard claim denials usually result in revenue loss and require an appeal to manage the claim.
- Preventable Denial – Preventable denial occurs when there are errors in registration, incorrect codes, or issues with insurance eligibility.
- Clinical Denial – Clinical denial is a hard denial that occurs when payment is not received for medical necessity, and an appeal is necessary to manage it.
- Administrative Denial – Administrative denial is a soft denial where the payer notifies the healthcare provider of the reason for the denied claim. But, the provider can file an appeal.

Steps To Prevent Claim Denials
Most denied claims are preventable, and simple operational process changes can save you time and money. Here are some of the best operational process changes to help you proactively prevent claim denials.
Educate and communicate – Communication is the key to success for any business. Front and back medical staff must understand their roles from patient check-in, documentation, clinical care, and collecting payments, including insurance plans, deductibles, and medical coding.
Verify insurance before services – Verifying insurance details is essential in preventing denied claims, particularly given the numerous factors that impact coverage. These factors include changes in employment, age, enrollment in Medicare, and fluctuation between commercial insurance plans. Even the same insurance can have different member IDs and coverage services year to year. The dealing staff must check insurance details before every visit and service required, just to be sure.
Know your payers – A payer also benefits in resolving denial issues, so it is essential to know and collaborate with your payers. Most providers accept insurance plans, and even similar programs have variations of allowable and reimbursable. It is a complex but vital area of denial management.
Having a good relationship with your payers will make understanding the rules of medical necessity, referrals, prior authorizations, and many others easier.
Proper documentation – This should include audits of registration, insurance verification quality, zero payment claims, and write-off adjustments. Proper documentation is critical nowadays, especially with the increasing complexity of coding.
Learn from previous mistakes and rejections – Improperly collected data can cause a denial claim. So, it’s essential to leverage information, including the payer ID list and insurance company, in your health record systems. Learning from previous mistakes and revising the process causing problems can prevent repeated claim denials and lower denial rates.
Embracing Constant Changes – Embracing the changes can be challenging but critical in today’s ever-evolving technological society. And it is more than true in the healthcare industry, especially in medical billing. You should be open to change in your practice for anything that can move the key components of the revenue cycle further.
Mitigating Losses
Completely eradicating claim denials in healthcare may only sometimes be achievable. Still, with a well-planned and proactive approach, healthcare providers can significantly reduce their impact on the financial bottom line. An effective strategy involves analyzing data and utilizing best practices to manage claim denials while incorporating automation and technology tools to streamline processes.
Healthcare providers face numerous challenges when it comes to managing claim denials. These can range from a lack of clear communication with insurance companies to inaccurate or incomplete patient information. Such challenges can lead to delays in processing claims, resulting in negative financial implications for providers. However, by analyzing data and identifying patterns and trends in claim denials in a timely manner, providers can implement evidence-based best practices to manage and reduce these denials.
Technology Solutions to Claim Denials
Effective management of claim denials in healthcare requires access to the appropriate technological resources. One such resource is claim editor or “claim scrubber” software that can process professional and institutional claims from the payer’s perspective. These software solutions leverage medical necessity databases to identify and double-check a comprehensive set of codes and capture significant complications that might have been missed in an extensive, complex medical record.
These solutions perform various edits, such as diagnosis code edits, medical necessity edits, procedure code edits, claim-level technical edits, outpatient prospective payment system (OPPS) edits, and file format edits. Diagnosis code modifications help to ensure that the codes reported on the claim align with the patient’s clinical condition and support medical necessity. Medical necessity edits help to identify services that are not medically necessary and are likely to result in denials. Procedure code edits help identify services bundled with other services and require additional documentation to support separate billing.
Access to appropriate technology resources and software can significantly improve the ability to fight claim denials in healthcare. These solutions can help to identify coding errors, missing documentation, and other issues that may result in claim denials, thereby reducing the financial impact on healthcare providers.
Hansei Solutions and Claim Denials
At Hansei Solutions, we understand healthcare organizations’ challenges when dealing with denied claims. That’s why we’re here to help. Our team of experts uses advanced technology and analytical systems to effectively manage claim denials to ensure that our clients get paid on time.
We provide medical billing solutions for behavioral health practices and ambulatory surgery centers and over the years have successfully handled thousands of claims, obtaining millions of dollars in reimbursements for our clients. Contact us to find out more.
Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.