Utilization Review With Hansei Solutions
Hansei Solutions is committed to providing utilization review services that assess the medical necessity, appropriateness, and efficiency of healthcare services to ensure they meet quality and cost standards, all while ensuring your clients receive the care and coverage they deserve.

Comprehensive Utilization Review Services
Hansei Solutions’ utilization review services prioritize you and your client’s best interests, promoting the placement of individuals in the least restrictive and least resource-intensive level of care necessary to meet their needs. These evidence-based methods are tailored to each provider’s unique participation criteria and standards, ensuring high-quality care for all demographics and diagnoses.
Our trained professionals handle all communication with payers regarding authorizations, allowing your clinical staff to focus on treating your clients without the distraction of managed care. We aim to obtain insurance coverage for your client’s entire health plan at the clinically indicated level of care designated by your treatment team, from initial payer approval to concurrent service reviews, appeals, and post-service reviews.
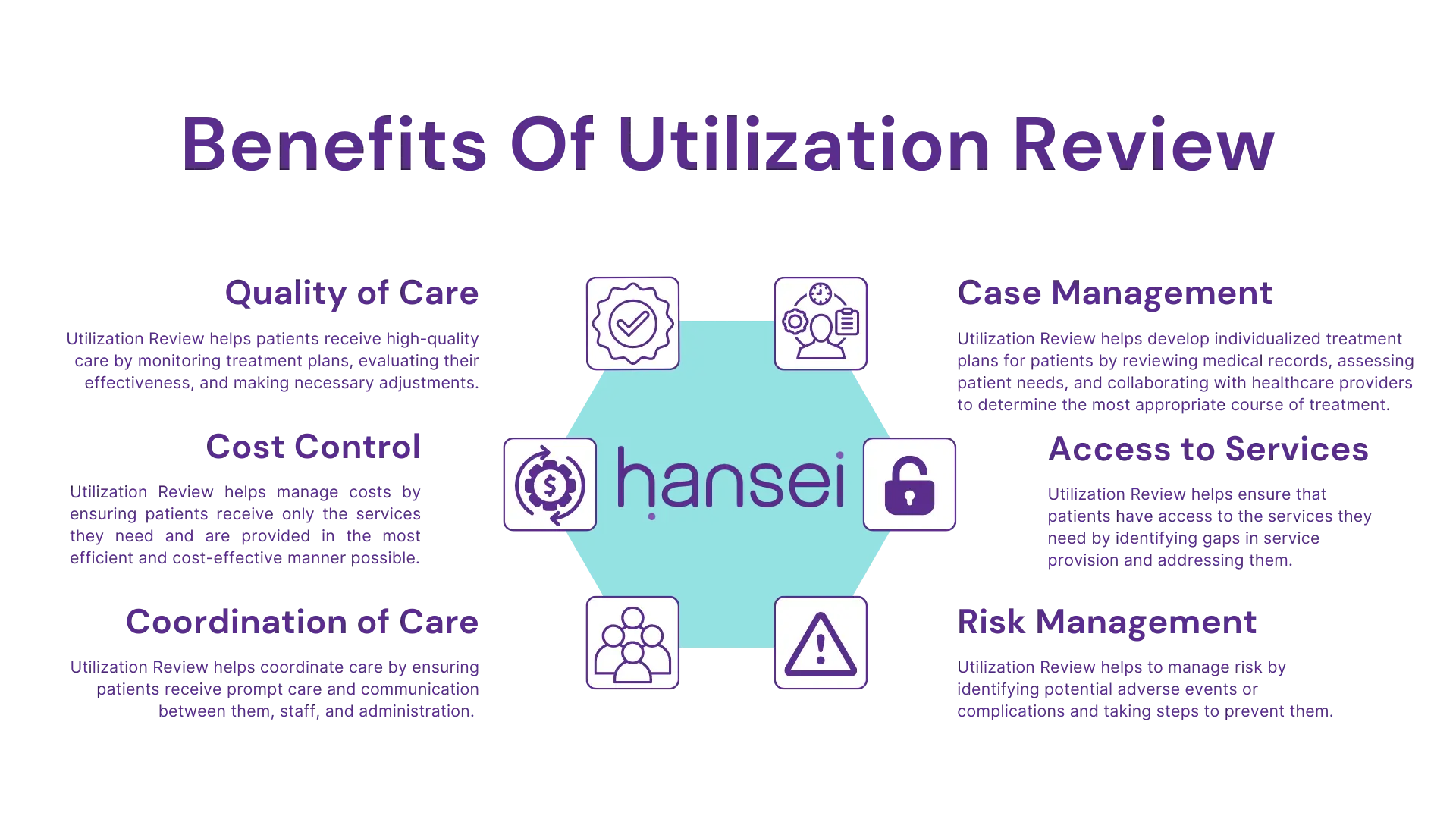
The Importance Of Utilization Review
According to data from the Organization for Economic Cooperation and Development (OECD), the United States spends nearly twice as much per capita on healthcare as the average of other developed countries. Utilization review plays a critical role in both addiction and mental healthcare, ensuring low costs and maximum revenue. Its importance lies in three key areas.
- Firstly, it helps to address the rise of behavioral healthcare costs by carefully evaluating the necessity and efficiency of procedures performed on patients. This ensures that insurance companies approve only legitimate claims and reduce unnecessary costs.
- Secondly, utilization review promotes better patient care by verifying the impact of procedures on their health. The findings can inform decision-making for similar treatments in the future, particularly for new or experimental medical treatments. This helps ensure patients receive the most appropriate care for their specific needs.
- Finally, utilization review helps to reduce the denial of claims by providing behavioral healthcare providers with valuable insights from procedure data. This enables providers to back up their claims and avoid denied claims, ensuring patients receive the care they need without unnecessary delays or complications.
Our Utilization Review Services
Our utilization review services streamline the behavioral healthcare decision-making process and surpass accreditation and state requirements, helping save valuable administrative and response time. Hansei Solutions’ utilization review services include:

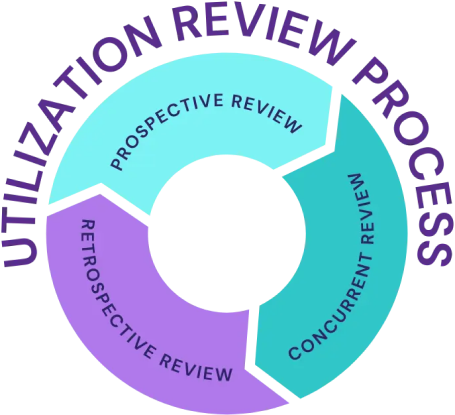
Our Utilization Management Process
Utilization management relies heavily on the review process, which encompasses three distinct types: prospective, concurrent, and retrospective. Each type involves a unique utilization review process flowchart with different use cases.

Prospective Review:
Prospective review is conducted before treatment to evaluate the procedure’s necessity and eliminate duplicate treatments. Other names for prospective review include prior authorization pre-service review, pre-procedure review, or pre-admission certification.

Concurrent Review:
This occurs while treatment is in progress to monitor the patient’s progress and resource utilization. This type is critical as insurance companies can deny coverage later on. Reviewers may also halt treatment prematurely or discharge patients earlier than anticipated. A concurrent review involves three significant areas: discharge planning, care coordination, and care transition.

Retrospective Review:
This is performed after treatment completion and focuses on effectiveness and appropriateness. The most important use of retrospective reviews is with claims, as they can be used to verify the accuracy of reimbursements and challenge denied claims.
Utilization Review Can Help
- Behavioral Healthcare: By monitoring and responding to effective treatment methods, Hansei Solutions can help addiction treatment centers provide the right care plans at the right time.
- Mental Healthcare: Utilization review can provide insight into the effectiveness of therapy types and healing modalities, ensuring they’re adjusted and explored as needed.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.