Blog
Credentialing in medical billing is a crucial step to ensure healthcare providers are qualified, experienced, and authorized to deliver healthcare services. It involves verifying their credentials, such as education, training, licensure, and experience. This process is essential for maintaining quality healthcare services and for providers to get reimbursed by insurance companies.
What is Credentialing?
Credentialing is a detailed process that confirms healthcare providers’ qualifications. It includes verifying their education, training, residency, licenses, certifications, and work experience. This process is typically done by healthcare facilities, insurance companies, and third-party credentialing agencies to ensure that providers meet the necessary standards to practice medicine.
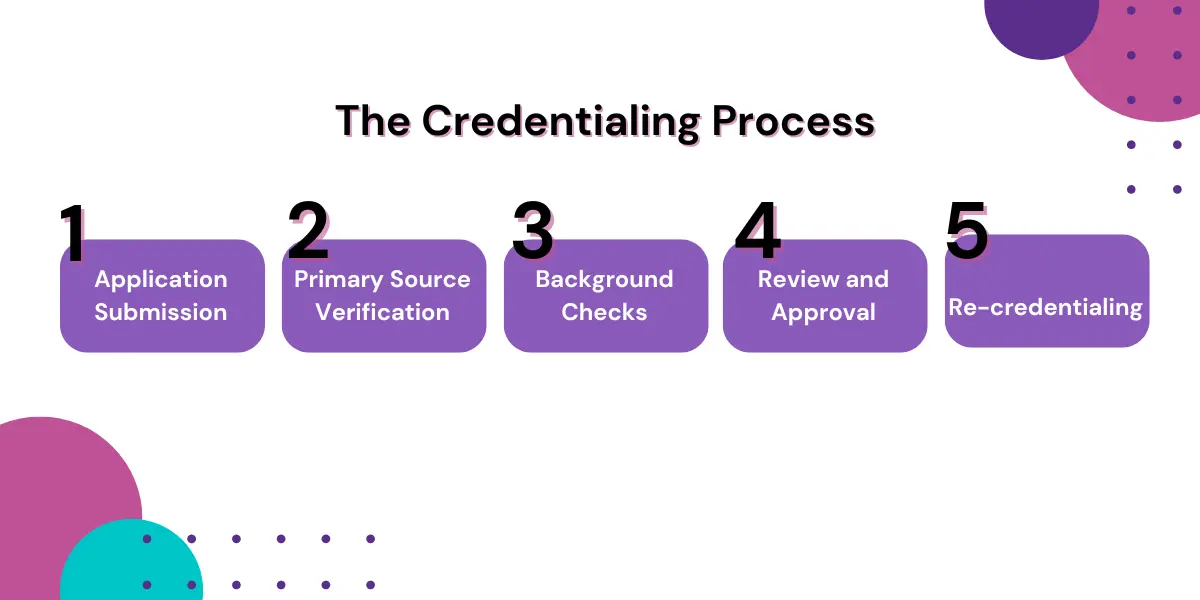
The Credentialing Process
The credentialing process is a critical step in ensuring that healthcare providers meet the necessary qualifications and standards to deliver quality care. This process involves verifying a provider’s education, training, experience, and professional licenses to confirm they are competent and qualified to practice. The credentialing process involves several steps:
- Application Submission: Healthcare providers submit an application to the credentialing body, which could be a hospital, insurance company, or credentialing agency. The application includes details about the provider’s education, training, licenses, certifications, work history, and professional references.
- Primary Source Verification: The credentialing body verifies the information provided through primary sources. This means contacting educational institutions, licensing boards, certification organizations, and previous employers to confirm the credentials are authentic.
- Background Checks: Comprehensive background checks are conducted to ensure that the provider has no history of malpractice, disciplinary actions, or criminal activity. This step is crucial for patient safety and trust.
- Review and Approval: The credentialing committee reviews the verified information and decides if the provider meets the necessary qualifications. If they do, the provider gets credentialed.
- Re-credentialing: Credentialing isn’t a one-time thing. Healthcare providers must go through re-credentialing periodically, usually every two to three years, to ensure they continue to meet the required standards and keep up with continuing education and training.
Why Credentialing Matters
Credentialing is a key part of healthcare that really makes a difference. It ensures that healthcare providers are qualified and capable of delivering the care patients need. By going through this process, healthcare facilities can maintain high standards, which helps reduce the chances of mistakes and malpractice. It also plays a big role in patient safety, as it prevents unqualified practitioners from getting involved in patient care, building trust between patients and their providers.
Credentialing is also necessary for meeting regulatory requirements and staying compliant with state, federal, and insurance company standards. It’s not just about ticking boxes—it’s what allows healthcare providers to join insurance networks and get reimbursed for their services. Without proper credentialing, providers might miss out on insurance coverage, which is a crucial part of running a healthcare business smoothly.

Challenges in Credentialing
While credentialing is essential in healthcare, it comes with its own set of challenges that can make the process complex and time-consuming. These hurdles often create obstacles for healthcare providers and organizations alike. Some of the most common challenges include:
- Lengthy Process: Credentialing can take several months due to the thorough verification and review required. This can delay the start of practice for new healthcare providers.
- Resource Intensive: Credentialing requires significant administrative resources, including personnel and time, to gather, verify, and review the necessary information.
- Variability in Standards: Different healthcare organizations and insurance companies may have varying credentialing standards and requirements, leading to inconsistencies and confusion.
- Technological Limitations: Many healthcare organizations still rely on manual processes for credentialing, which can be inefficient and prone to errors. Adopting electronic credentialing systems can help streamline the process.
Despite these challenges, overcoming them is crucial to ensuring that healthcare providers are properly credentialed and ready to deliver quality care. By addressing these issues, healthcare organizations can make the credentialing process smoother and more effective.
How to Improve the Credentialing Process
To make credentialing easier and more efficient, healthcare organizations can try a few practical approaches. One of the best ways is to adopt automated systems. By switching to electronic credentialing, the whole process becomes quicker and less prone to errors. These systems can take care of collecting, verifying, and tracking credentials, making everything run more smoothly. Another helpful move is to standardize credentialing procedures across different organizations and insurance companies, which can cut down on confusion and keep things consistent.
Collaboration is also key. By working together with credentialing agencies and sharing information, healthcare organizations can make the process more efficient. Additionally, using continuous monitoring and real-time verification can help ensure that healthcare providers stay up-to-date with their credentials and meet ongoing requirements. These strategies can help healthcare organizations tackle the common hurdles in credentialing and make the process much more manageable.
A More Efficient Credentialing Process with Hansei
Credentialing in medical billing is a key process that makes sure healthcare providers are qualified, competent, and authorized to deliver care. It’s essential for maintaining high-quality care, patient safety, and staying compliant with regulations. While the credentialing process can be challenging, it can be made easier with the right tools, such as automated systems, standardization, teamwork, and ongoing monitoring. By improving how credentialing is done, healthcare organizations can boost efficiency and effectiveness, benefiting both providers and patients.
If you’re looking to simplify and strengthen your credentialing process, Hansei Solutions can help. Let’s work together to make sure your team is set up for success.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.