Blog
Denial management in medical billing is the structured process of identifying, resolving, and preventing insurance claim denials to ensure healthcare providers receive the revenue they’ve earned. With denial rates ranging from 5% to 17% and up to 65% of denied claims never reworked, effective denial management is vital for maintaining cash flow, reducing revenue loss, and improving operational efficiency. At Hansei Solutions, this process includes early detection, categorization of denial reasons, root cause analysis, resolution through corrections or appeals, and long-term prevention strategies. Technology plays a key role by flagging errors, analyzing trends, and tracking appeal deadlines. Without strong denial management, practices risk lost revenue, increased administrative costs, and patient dissatisfaction—making it a crucial part of a healthcare organization’s financial health and sustainability.
What is Denial Management in Medical Billing?
In medical billing, few challenges are more costly or frustrating than claim denials. Denial management in medical billing is the structured process of identifying, resolving, and preventing insurance claim denials so healthcare providers receive the revenue they’ve earned.
At Hansei Solutions, we know that each denial not only delays payment but also strains cash flow, affects operations, and can even disrupt patient care. Denial management isn’t just an administrative task—it’s essential for maintaining financial health and stability in any healthcare organization.
Why Denial Management Matters
Industry estimates show that denial rates can range between 5% and 10%, going as high as 17%, though some practices face even higher rates. Denials consume time, drain resources, and ultimately threaten a practice’s bottom line. Alarmingly, about 65% of denied claims are never reworked, leading to permanent revenue loss.
Effective denial management offers clear benefits. It helps recover revenue that might otherwise be lost, reduces the average number of days claims spend in accounts receivable, and improves operational efficiency. Equally important, it helps pinpoint recurring issues that cause denials, paving the way for long-term solutions and fewer headaches down the line.
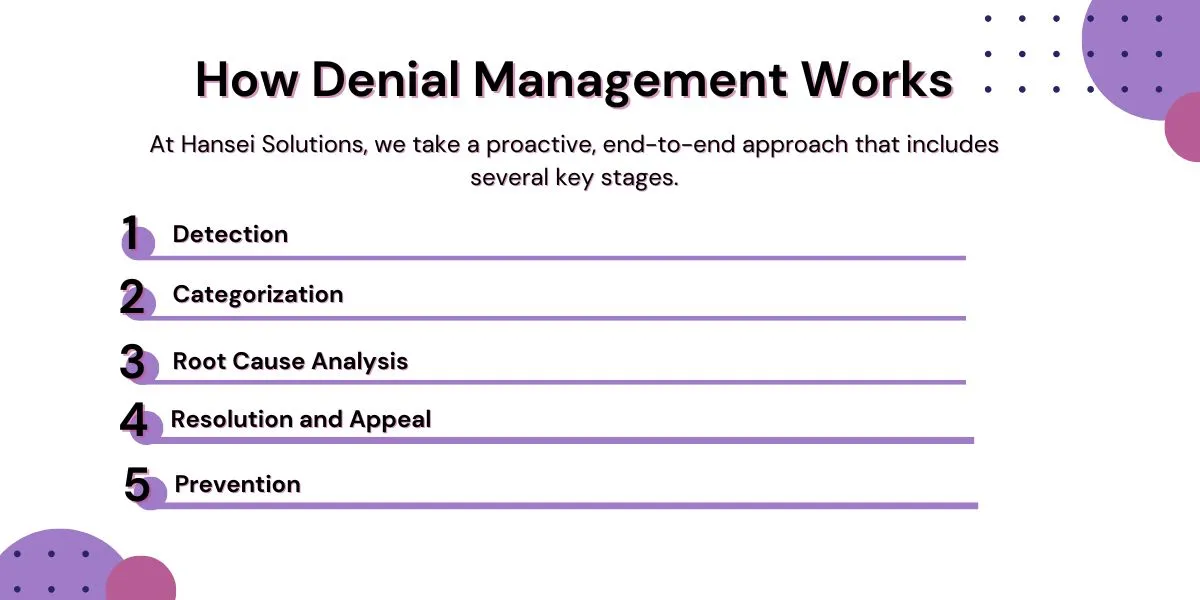
How Denial Management Works
At its core, denial management is more than just fixing claims—it’s about transforming processes to stop denials from happening in the first place. At Hansei Solutions, we take a proactive, end-to-end approach that includes several key stages.
Detection
The first step is spotting denials quickly. Many practices rely on notifications from clearinghouses or practice management software to flag denied claims the moment they’re returned by payors. Prompt detection is critical because time limits for appealing denials are strict and vary by insurer.
Categorization
Not all denials are created equal. Identifying the reason behind each denial helps streamline the path to resolution. Denials might stem from administrative errors like missing patient details, or clinical issues such as questions over medical necessity.
Some of the common categories include:
- Missing or incorrect patient information
- Authorization or referral issues
- Coverage exclusions or policy limitations
- Coding errors or mismatches
- Duplicate claims
- Timely filing violations
Understanding these categories helps denial management teams prioritize and respond efficiently.
Root Cause Analysis
Simply correcting a claim and resubmitting it isn’t enough. Hansei Solutions focuses on identifying why denials occur in the first place. For instance, we might discover recurring errors in patient demographics collection at the front desk, confusion over prior authorization requirements for specific services, or gaps in communication about new coding updates.
Finding and fixing root causes is what transforms denial management from reactive problem-solving into proactive revenue protection.
Resolution and Appeal
Once we determine the cause, the next step is correcting the claim and resubmitting it. In more complex cases—like disputes over medical necessity—we handle formal appeals, gathering supporting medical records and documentation to present the strongest case possible.
Appeals can be time-sensitive, with strict deadlines and unique requirements for each payor. Hansei Solutions ensures all appeals are thorough, timely, and compliant with insurer guidelines, increasing the chances of overturning denials and recovering revenue.
Prevention
Perhaps the most critical part of denial management is prevention. At Hansei Solutions, we analyze denial patterns to help providers make long-term changes. Prevention strategies might involve updating staff training, adjusting workflows, or implementing new billing checks to reduce errors before claims are even submitted.
Technology’s Role in Denial Management
Modern denial management increasingly relies on technology to boost efficiency and accuracy. Advanced revenue cycle management (RCM) systems can:
- Flag potential errors before claims go out
- Analyze denial trends to identify recurring issues
- Provide real-time dashboards showing denial rates by payor, service line, or department
- Send alerts to ensure appeals are filed within required timeframes
At Hansei Solutions, we integrate powerful RCM technology with expert human oversight. This combination helps us detect issues faster, reduce error rates, and keep our clients’ revenue flowing smoothly.
The Cost of Ignoring Denials
Ignoring denials can have significant consequences. Practices without robust denial management often face permanent revenue loss, higher days in A/R, and cash flow interruptions. Patients may also experience frustration from unexpected bills or delayed services.
The American Medical Association estimates the average cost to rework a denied claim at around $25. When multiplied across hundreds—or even thousands—of claims, the financial stakes become clear. Denial management isn’t just an administrative task; it’s a critical investment in a practice’s sustainability and growth.
Frequently Asked Questions About Denial Management
What are the most common reasons for claim denials?
Some of the top reasons claims are denied include missing or incorrect patient information, lack of prior authorization, services not covered by the patient’s insurance, coding errors, duplicate submissions, and submitting claims past payor deadlines.
How long does it take to resolve a denied claim?
The timeline varies depending on the denial’s cause and the payor involved. Simple issues might be resolved in a few days, while complex appeals—such as disputes over medical necessity—can take several weeks or even months. Prompt action and thorough documentation are key to resolving denials quickly.
Is it worth appealing denied claims?
Absolutely. Many denied claims are recoverable through appeals, especially when denials result from administrative or documentation errors. Studies suggest that over 50% of denied claims may be overturned with proper follow-up, so pursuing appeals is often well worth the effort.
How can providers prevent denials?
Prevention strategies include verifying insurance eligibility before services are rendered, training staff on accurate coding and documentation, staying up to date on payor rules, and using technology to catch errors before claims go out. Partnering with denial management experts like Hansei Solutions can make a significant difference.
How does denial management improve patient satisfaction?
When billing errors and denials are minimized, patients receive clearer, more accurate bills and face fewer unexpected costs. This leads to a better overall experience, increased trust, and higher patient satisfaction.
How Hansei Solutions Can Help with Denial Management
At Hansei Solutions, denial management is at the heart of our revenue cycle services. We specialize in helping behavioral health providers and other complex healthcare organizations navigate the unique challenges of insurance billing. Our approach blends industry expertise with powerful technology and a commitment to proactive solutions.
We’re here to help you protect your revenue, enhance compliance, and keep your operations running smoothly—so you can focus on what matters most: patient care.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.