Blog
When it comes to medical billing, especially for Medicare claims, there are a lot of terms and processes that can seem confusing. One term you may hear often is MAC, short for Medicare Administrative Contractor. These organizations play a vital role in keeping the Medicare system running smoothly and making sure providers get reimbursed for the services they provide.
What is a Medicare Administrative Contractor (MAC)?
A Medicare Administrative Contractor is a private organization that acts as a bridge between healthcare providers and the Centers for Medicare & Medicaid Services (CMS). Essentially, MACs manage Medicare claims for Parts A and B (hospital insurance and medical insurance) and Durable Medical Equipment (DME). They handle the nitty-gritty details of claims processing, provider enrollment, medical reviews, and appeals.
MACs are contracted by CMS to ensure that claims are processed accurately and efficiently. They cover specific regions or jurisdictions in the U.S., which means providers in different states may work with different MACs. This structure helps streamline the processing of millions of claims while maintaining compliance with Medicare guidelines.
According to the latest data from CMS, there are 12 A/B MACs and 4 DME MACs managing claims for over 35 million Medicare beneficiaries. These beneficiaries account for about 54% of the total Medicare population.
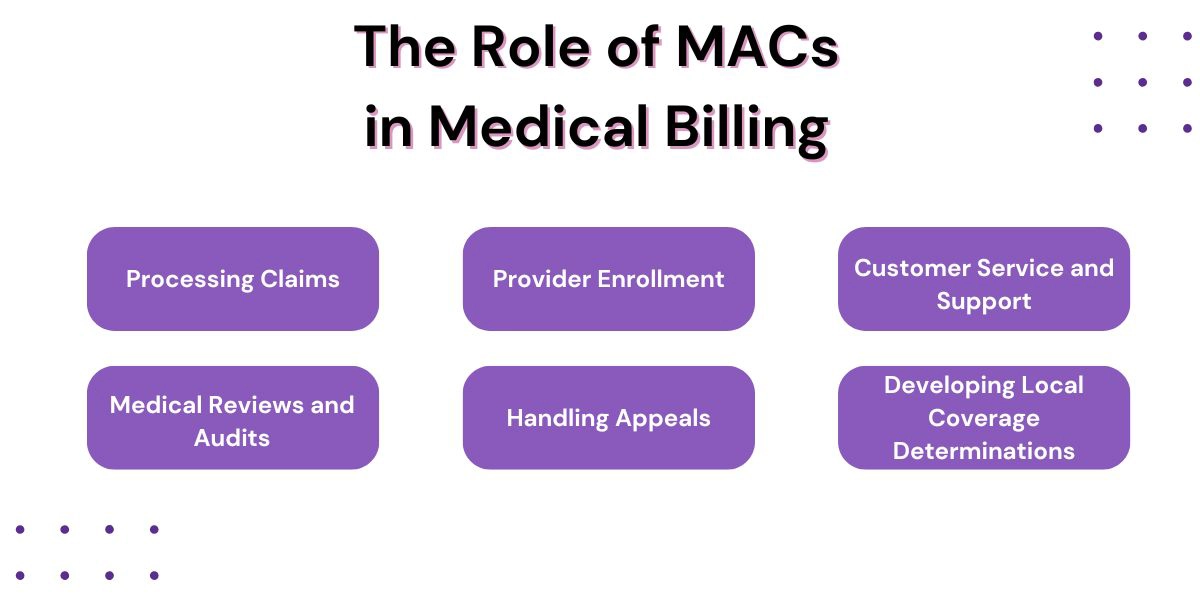
The Role of MACs in Medical Billing
So, what exactly do MACs do? Their responsibilities are more extensive than you might think:
1. Processing Claims
MACs handle the review and payment of Medicare fee-for-service (FFS) claims. When a healthcare provider submits a claim, the MAC verifies that the claim meets Medicare’s coverage requirements and that the services provided are accurately coded. This step is crucial in ensuring that Medicare funds are used appropriately.
2. Provider Enrollment
Before a healthcare provider can bill Medicare, they need to be enrolled in the program. MACs manage this process, making sure providers meet all qualifications and follow Medicare’s rules. This helps maintain the integrity of the Medicare system by preventing fraudulent providers from participating.
3. Customer Service and Support
MACs act as the main point of contact for both providers and beneficiaries. If a provider has questions about a claim or a patient needs clarification about coverage, the MAC is there to help. They offer education and guidance to ensure everyone stays informed about the latest Medicare policies and updates.
4. Medical Reviews and Audits
To prevent fraud and improper payments, MACs perform medical reviews of claims. This involves checking medical records to make sure services were medically necessary and billed correctly. In 2021, improper Medicare payments totaled around $25 billion, highlighting the importance of these reviews.
5. Handling Appeals
When a claim is denied, providers or patients can file an appeal. MACs handle the first level of appeals, known as redeterminations. This process ensures that providers have a fair opportunity to contest denied claims.
6. Developing Local Coverage Determinations (LCDs)
MACs also create Local Coverage Determinations (LCDs), which define which services are considered reasonable and necessary in their specific region. These guidelines help providers understand what Medicare will and won’t cover.
How MACs are Structured by Region
The U.S. is divided into jurisdictions for A/B and DME claims, and each jurisdiction is assigned a MAC. For example:
- Jurisdiction J covers Alabama, Georgia, and Tennessee and is managed by Palmetto GBA.
- Jurisdiction M covers North Carolina, South Carolina, Virginia, and West Virginia and is also managed by Palmetto GBA.
- Jurisdiction F covers Alaska, Arizona, Idaho, Montana, North Dakota, Oregon, South Dakota, Utah, Washington, and Wyoming and is managed by Noridian Healthcare Solutions.
Knowing your MAC is crucial for understanding who to contact for claims issues and updates.
Why MACs Matter to Healthcare Providers
For healthcare providers, MACs are essential partners in the medical billing process. By ensuring claims are processed correctly, MACs help providers receive timely and accurate payments. They also offer training, resources, and updates to keep providers informed about changes in Medicare policies.
Challenges Providers Face When Working with MACs
While Medicare Administrative Contractors (MACs) play an essential role in medical billing, providers often encounter challenges that complicate claims processing and compliance. Here are some common issues and how to address them:
- Differences in Processing: Each MAC may interpret Medicare guidelines slightly differently, leading to inconsistencies in how claims are handled. A claim approved in one region might be denied in another.
Solution: Stay informed about your MAC’s specific Local Coverage Determinations (LCDs) and communicate regularly with their support team for clarification. - Frequent Policy Changes: Medicare rules and coding guidelines change frequently. Missing updates can result in errors or denied claims.
Solution: Subscribe to your MAC’s email alerts and attend educational webinars. Regularly train your billing staff on the latest Medicare policies. - Appeals Backlogs: Due to high claim volumes, the appeals process can be slow, impacting cash flow. In 2021, over 870,000 appeals were pending.
Solution: Submit accurate claims to avoid denials and track appeals using billing software that automates follow-ups. - Communication Barriers: Long wait times for customer support can hinder problem resolution.
Solution: Assign a billing liaison in your practice to handle MAC interactions and use self-service portals to track claims. - Technological Challenges: Outdated systems can lead to submission errors.
Solution: Invest in modern billing software compatible with MAC systems and utilize MAC-provided technical resources.
Overcoming these challenges requires staying informed, leveraging technology, and maintaining strong communication with your MAC.
Get Medical Billing Help From Hansei Solutions
Managing the processes of behavioral health medical billing on your own can be overwhelming, especially with frequent policy changes and the risk of claim denials. That’s where Hansei Solutions comes in. We provide expert medical billing services to help your practice stay compliant, minimize denials, and streamline reimbursements.
Don’t let medical billing complexities slow you down. Contact Hansei Solutions today to discover how we can optimize your billing processes and let you focus on what matters most: delivering excellent patient care.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.