Blog

Table of Contents
When it comes to having a successful medical practice, there are a lot of elements to consider and Revenue cycle management (RCM) is one of the most critical. RCM enables healthcare providers to receive prompt payment for the services that they provide. Not only does this benefit the provider, but it also has advantages for the patient. Read on to find out more about RCM and why it is so crucial.
Revenue cycle management (RCM) is an organization’s financial monitoring process that is used to recognize and oversee incoming payments. This allows businesses to ensure a degree of transparency and is important in making sure that patients are billed the accurate amount for the care and services they have received.
What is Revenue Cycle Management?
Revenue cycle management is a system healthcare facilities employ to manage their administrative and medical operations connected to the income process. The revenue cycle commences when a patient gets in touch to arrange a meeting and comes to an end when all payments for the visit and the treatment are accumulated. The purpose of revenue cycle management is to identify and address any problems that may be preventing the provider from getting full reimbursement and thus, increasing their income. With the right strategy, healthcare providers can attain the highest possible reimbursement and improve their revenues.
Revenue Cycle Management Stages
The healthcare revenue cycle is a multifaceted process that involves a lot of steps, and this opens up the potential for mistakes to happen. These missteps can delay or even stop the reimbursement that providers receive from insurance companies and patients. In order to have a better idea of where errors may occur and how revenue cycle management (RCM) can address them, let’s have a look at the stages of the healthcare revenue cycle.
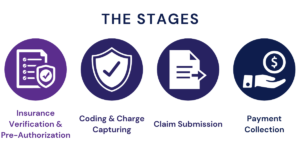
Stage 1 – Insurance Verification and Pre-Authorization
When a person seeks medical care, the healthcare provider must gather important information to open a patient record. This information includes the patient’s insurance coverage details and verifying if their insurance policy is valid. Revenue cycle management stresses the importance of correctly entering this information, even if the patient has already been seen at the provider’s practice. An incorrect or invalid insurance policy can result in a declined claim later on in the revenue cycle, which causes a postponement of the provider’s reimbursement and additional work for the provider to identify and rectify the mistakes that were made.
Stage 2 – Coding and Charge Capturing
The act of charge capturing is the transcription of services done for a patient into charges that use a globally accepted medical coding system. These codes are used to determine how much an insurer will reimburse. If the coding is incorrect, the claim of the patient may be declined. This leads to a stalled payment to the provider and also causes the provider to spend extra time and money to look into the denied claim and make an appeal. To make sure that rejections do not happen, proper revenue cycle management is necessary to guarantee that the coding is accurate.
Stage 3 – Claim Submission
When a patient receives care, the charges are documented and coded, and then a claim is sent to the insurance provider. The cost is determined by the predetermined amounts for the medical codes included in the claim. If the claim is filled out appropriately, the insurance company should be able to quickly process the payment. However, if mistakes are made, the insurer may return the claim to the hospital or doctor’s office to be filled out again. To prevent payment postponements, the claim should be inspected by a software program or a billing/coding expert. They are able to recognize and fix any errors before sending the claim to the insurance agencies.
Stage 4 – Payment Collection
After the application for coverage by the patient has been accepted, the insurance business gives back money to the service provider in line with the patient’s qualifications. In the event that there is still an outstanding balance following the insurance repayment, the service provider is responsible for getting in touch with the patient to secure the remaining payment.
Benefits of Revenue Cycle Management in Healthcare
Revenue Cycle Management is designed to guarantee that all related steps are carried out accurately and completely so that service providers can prevent any potential postponements or loss of revenue. The primary target of RCM is to raise revenue for providers, though it also offers other advantages. These advantages are not only of benefit to providers but also to patients, making revenue cycle management even more valuable. Revenue cycle management benefits include:

Identify Errors
Implementing RCM allows healthcare providers to recognize where problems are occurring in the revenue cycle. This helps to reduce the probability of claim rejections since almost 90% of them are caused by problems that can be easily prevented, such as not having all the necessary information in the patient’s records or using the wrong coding. If these mistakes are avoided and claims are accepted upon first submission, providers are able to receive their reimbursements much quicker. Plus, they don’t have to use extra resources to investigate and appeal any rejected claims. On average, hospitals can make an extra $5 million in income by preventing claim denials. This fact alone should be sufficient grounds for healthcare providers to consider how they can improve their revenue cycle management.
Prevent Healthcare Fraud
RCM offers the advantage of preventing healthcare fraud and abuse, which is a huge problem for the healthcare sector, resulting in billions of dollars of losses each year. Besides, a fraud inquiry can bring about a decrease in revenue and a deterioration of a provider’s reputation. Inaccurate coding, either deliberate or unintended, can also lead to probes for fraud. Furthermore, providers may demand a higher reimbursement rate for services that don’t require it, which is known as upcoding. By ensuring accurate data collection, billing, and coding, RCM reduces the chances of providers submitting false information to insurers. Moreover, RCM keeps providers aware of the ever-altering healthcare guidelines, thereby averting unintentional fraud.
Decrease the Burden on Administration
When denials are kept to a minimum, the workload of administrative staff is reduced. This means they can dedicate more attention to patient care. Moreover, with a concentrated effort on tasks such as appointment setting, filling out intake forms and collecting payments, interactions between staff members and patients are made smoother, creating a more pleasant experience for everyone.
Increase the Facility’s Revenue
Healthcare providers can have their services immediately reimbursed by avoiding mistakes in their paperwork, rejected claims, and any kind of fraud. Additionally, they can save a lot of money that would otherwise have to be spent on correcting errors, making appeals, and dealing with any fraudulent activities. With the extra money they gain, they are able to invest more in their patient care. Ultimately, their main focus is to provide excellent care to their patients.

What Makes Revenue Cycle Management Important?
Apart from delivering the most excellent care, an effective revenue cycle management (RCM) is crucial for an organization’s financial stability. A strong and successful healthcare RCM ensures timely income, consistent payments, and monetary sustainability for organizations, allowing them to concentrate on offering quality care to patients. RCM is distinctive to each organization and its capacity to efficiently handle medical billing and revenue.
Regardless of size, from small clinics to large healthcare systems, the aim is the same: maximize income and reduce debt and expenses. To accomplish this, both the patient’s healthcare team and the organization’s administrative team must be in agreement. Nowadays, customers expect a smooth and connected experience, from the time they book an appointment or walk into a healthcare center to when they receive their invoice. This necessitates that teams collaborate to make sure that the revenue cycle management (RCM) process is as efficient as possible.
Every step, such as capturing charges, presenting the claim, coding, collecting payments from patients, registering, processing reimbursements, chasing third parties, and analyzing usage, all have an effect on the speed of revenue and the overall fiscal wellness of the organization.
Revenue Cycle Management at Hansei Solutions
Regardless of what stage your business is in, Hansei Solutions offer a complete set of revenue management services to address issues and maximize opportunity. From daily business operations such as estimating a customer’s out-of-pocket costs and scrutinizing medical billing procedures to utilizing advanced technologies to furnish your firm with predictive analytics and compliance information, we help you get paid quicker, predict revenue, and make more educated business decisions.
We know it requires commitment, constant creativity, and responsiveness to build connections and, ultimately, grow your business. We at Hansei Solutions, are devoted and in it for the long haul. We are here to address all issues and create growth opportunities for your organization. We are passionate about what we do, and it reflects in every interaction we have. Learn more about Hansei Solutions and how we can help you by contacting us today.

Download Our FREE eBook

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.