Blog

Utilization review (UR) in healthcare is a structured process used to assess the medical necessity, appropriateness, and efficiency of care before, during, and after treatment. It acts as a checkpoint between healthcare providers and insurers, aiming to control costs while ensuring patients receive the right level of care. UR is critical for both patient outcomes and provider revenue, as claim denials often stem from insufficient documentation or unmet medical necessity criteria. The process includes prospective (pre-authorization), concurrent, and retrospective reviews, each with unique requirements and challenges such as administrative burden, care delays, and varying insurer standards. At Hansei Solutions, UR is seen as vital to the revenue cycle, and they support providers with tailored strategies and technology to reduce denials, streamline documentation, and improve authorization success rates—ultimately safeguarding both patient care and financial performance.
What is Utilization Review in Healthcare?
Healthcare is complex, both clinically and financially. Providers aim to deliver the best care for patients—but payors want to ensure those services are medically necessary and cost-effective. This is where utilization review (UR) comes in.
Utilization review in healthcare is the systematic process of evaluating the medical necessity, appropriateness, and efficiency of healthcare services before, during, or after patient care. It acts as a checkpoint between providers and insurance payors, helping control healthcare costs while safeguarding patients from unnecessary treatments.
At Hansei Solutions, we view utilization review as a critical piece of the revenue cycle puzzle. For behavioral health providers and other specialties delivering high-cost services, effective UR can mean the difference between claims being paid smoothly or denied altogether.
Why Utilization Review Matters
Healthcare spending in the U.S. reached nearly $4.5 trillion in 2022, according to the Centers for Medicare & Medicaid Services (CMS). With such high costs, insurers rely on utilization review to manage spending and ensure that treatments align with established standards of care.
While UR serves the goal of preventing unnecessary services, it also directly impacts providers’ revenue. A lack of proper documentation or failure to meet specific medical necessity criteria can lead to claim denials—even when the service provided was clinically appropriate.
Effective utilization review helps:
- Ensure patients receive appropriate levels of care
- Prevent costly and avoidable treatments
- Reduce insurance denials related to medical necessity
- Maintain compliance with payor requirements
- Improve cash flow and revenue cycle performance
For providers, UR is both a clinical safeguard and a financial necessity.
How Utilization Review Works
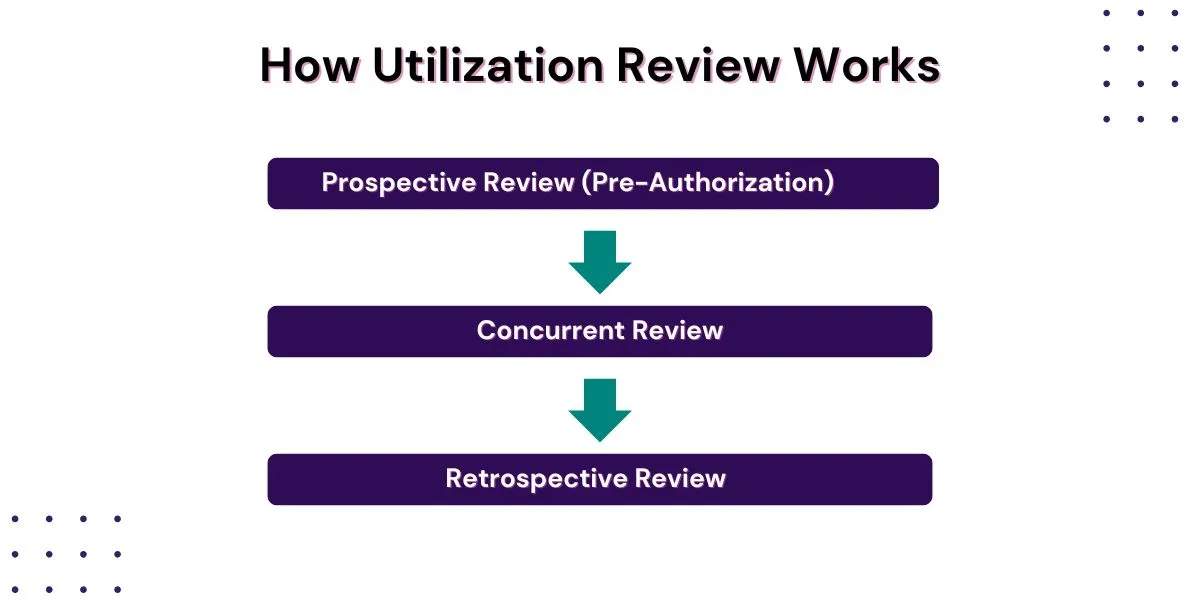
Utilization review isn’t a single event—it’s a series of evaluations that can occur at multiple points during a patient’s care journey. At Hansei Solutions, we help clients navigate each stage of UR to protect revenue and ensure compliance.
Prospective Review (Pre-Authorization)
This first stage happens before services are delivered. Insurers require providers to submit detailed clinical information explaining why a specific treatment, test, or level of care is necessary. Without pre-authorization, providers risk delivering services that insurers later refuse to cover.
Concurrent Review
While a patient is receiving care, concurrent reviews assess whether continued treatment remains medically necessary. Utilization reviewers—often nurses or physicians working for insurance companies—evaluate progress notes, therapy updates, and discharge plans.
These reviews can result in:
- Approval for continued treatment
- Recommendations to step down to a lower level of care
- Requests for additional documentation to justify ongoing services
Timely and thorough communication during concurrent reviews is essential to avoid disruptions in patient care and prevent denied days of coverage.
Retrospective Review
After services are provided, payors may conduct retrospective reviews to confirm medical necessity and adherence to treatment guidelines. Even if prior authorizations were obtained, retroactive audits can still result in recoupment demands if documentation is incomplete or inconsistent.
Challenges in Utilization Review
While UR serves an important purpose, it often creates significant challenges for providers:
- Administrative Burden – Collecting documentation, responding to reviewers, and navigating insurer portals consume valuable staff time.
- Varying Payor Requirements – Each insurance company has unique medical necessity criteria, making it difficult for providers to keep up.
- Potential Care Delays – When UR decisions are delayed, patients may wait for necessary treatment, creating frustration and clinical risks.
- Denials and Revenue Loss – Even small gaps in documentation can lead to denied claims and lost revenue.
At Hansei Solutions, we specialize in helping practices manage these challenges. Our goal is to reduce administrative stress while improving authorization success rates and protecting revenue.

Technology’s Role in Utilization Review
Technology can make utilization review more efficient and less prone to error. Electronic health records (EHRs), integrated RCM systems, and UR-specific software tools help:
- Generate required reports and treatment summaries
- Track authorization deadlines and follow-up tasks
- Standardize documentation to meet payor criteria
- Identify trends in denials related to medical necessity
However, technology alone isn’t enough. Skilled professionals are essential for crafting strong clinical narratives, understanding medical necessity criteria, and communicating effectively with payors.
At Hansei Solutions, we combine advanced technology with deep industry expertise to manage UR proactively and efficiently.
The Cost of Poor Utilization Review
Failing to manage utilization review effectively can have severe consequences for providers, including:
- Lost revenue from denied claims
- Increased write-offs due to lack of documentation
- Disruptions in patient care when services are delayed or denied
- Higher administrative costs from repeated appeals and rework
Industry data suggests that denials related to medical necessity account for a significant portion of all denied claims. The American Medical Association reports that about 9% of all claims face prior authorization hurdles, with many leading to treatment delays or denials.
Frequently Asked Questions About Utilization Review
Is utilization review required for all medical services?
Not all services require utilization review, but many high-cost or high-risk procedures—such as inpatient admissions, residential treatment, or advanced imaging—typically do. Requirements vary significantly by payor.
How long does it take to get pre-authorization?
Timelines vary by insurer and service type. Some pre-authorizations can be granted in hours, while others may take days or longer. Prompt submission of thorough clinical documentation speeds up the process.
Can services be denied even after pre-authorization is granted?
Unfortunately, yes. A pre-authorization is not a guarantee of payment. Services can still be denied retrospectively if the payor determines that documentation does not support medical necessity or if discrepancies exist in records.
What’s the biggest reason services get denied during UR?
One of the most common reasons is insufficient documentation. Missing details about patient symptoms, lack of treatment progress notes, or failing to show why lower levels of care are inappropriate often result in denials.
How can providers improve utilization review outcomes?
Providers can improve UR results by training staff on documentation standards, maintaining detailed clinical records, using technology to manage deadlines, and working with experienced partners like Hansei Solutions who specialize in navigating complex payor requirements.
How Hansei Solutions Supports Utilization Review
At Hansei Solutions, we help behavioral health providers and other specialty practices navigate utilization review with confidence. Our services include:
- Assistance with obtaining timely pre-authorizations
- Support for concurrent reviews and communication with payors
- Detailed record audits to ensure readiness for retrospective reviews
- Staff training on payor-specific documentation standards
- Appeals support for denied services
Our proactive approach helps providers secure necessary authorizations, reduce denials, and keep revenue flowing smoothly. Contact us today to learn more about how Hansei Solutions can help your behavioral health practice with utilization review.

Ready to focus on providing healthcare? Let us lighten your load.
We’re here to address your pain points and create growth opportunities for your organization. We’re passionate about what we do, and it shows in every interaction. Learn what makes us tick and schedule a demo today.